“You were speaking our language like no one else has before. We felt heard and like someone else understood our challenges for the first time.”
Those were the words a dad shared with me during our consultation all the way back 10+ years ago when I wrote my very first article on Sensory Integration Disorders for a local magazine. Not only had they met very few practitioners at that time who had even heard of Sensory Integration Disorder, but who also really understood that it was a significant challenge that negatively affected the quality of life of their child day in and day out.
Thankfully, we could give these parents, and this child, more explanation and information on what was causing the Sensory Integration Disorder, challenges in their son. We also created a very thorough action and care plan designed to help vastly improve their quality of life by addressing the sensory issues all the way to their root.
What Are Sensory Integration Disorders?
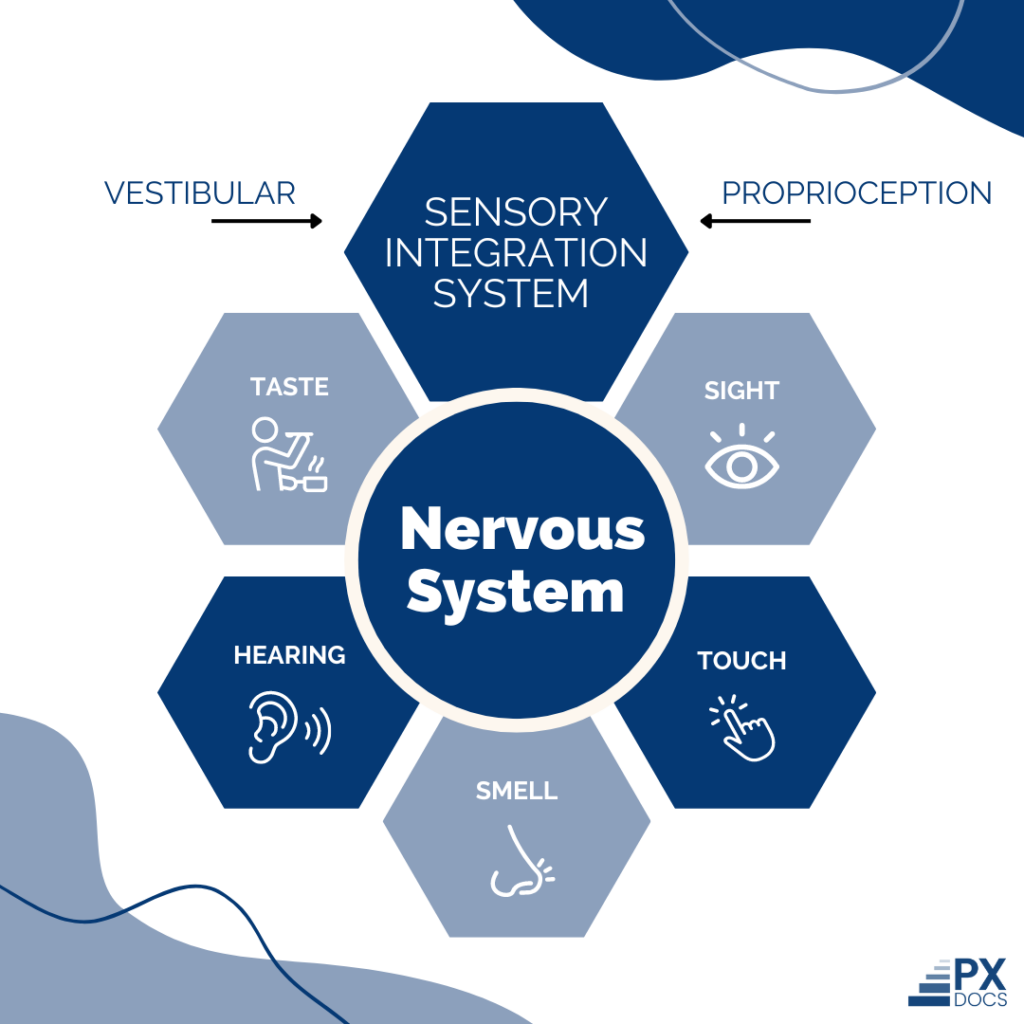
The nervous system is responsible for receiving and processing sensory information, and this process is more formally known as sensory integration. Sensory Integration Disorders (SID), also often referred to as Sensory Processing Disorders (SPD), are a type of condition where the brain struggles to process stimulation via the senses properly.
Leading specialist and neuroscientist A. Jean Ayres, Ph.D., suggests that sensory disorders like these are similar to a “neurological traffic jam” that ultimately prevents sensory information from being processed and sent where it needs to go. This can affect how children (and adults) regulate behavior, perform motor functions, and go about many other day-to-day activities.
When we say sensory information, we mean anything our bodies detect with one of our senses, like taste, touch, smell, hearing, and sight. There are also two “internal” senses that specialists associate with body awareness (proprioception) and movement (vestibular).
One tricky element of sensory processing disorders is that everyone can be affected differently. Some people are overstimulated, and even the most common noises or lightest touches can be uncomfortable or even painful. On the other hand, some people struggle to fully understand or sense stimulation, potentially making them uncoordinated or spatially unaware.
Sensory integration and learning disorders are usually identified during childhood, but they can be identified in adults, too. Note that the traditional medical industry currently doesn’t view sensory integration disorders as a legitimate diagnosis; instead, medical professionals often relate symptoms to other conditions.
Symptoms vs. Causes
Some people will have some kind of sensitivity to a specific sense, like loud noises, and others will be affected by multiple. Again, kids can be over- or under-sensitive to stimuli, and both sides of that spectrum come with challenges and frustrations.
What Are the Symptoms of Sensory Integration Disorder?
Overstimulated scenarios or behaviors in kids can look like this:
- Clothes being too itchy
- Sounds being too loud
- Lights are too bright
- Screaming or negatively responding when they’re touched
- Gagging due to food textures
- Vomiting in response to certain sounds, textures, or smells
- Soft touches feel too hard
- Reacting extremely to sudden movements
- Poor balance or clumsiness
- Poor motor skills, like writing with a pencil
Kids that are under-stimulated will often engage in sensory-seeking behaviors, which can look like this:
- Antsy or have trouble sitting still
- Don’t pick up on social cues or personal space
- Thrill-seeking behaviors, like jumping from heights or spinning
- Don’t get dizzy while spinning
- Don’t respond to extreme temperatures
- Wants visual stimulation (like video games or other electronics)
- Chews on things
- Don’t recognize when their face is dirty
- Have a high pain threshold
- Don’t always understand their own strength
Other symptoms include low muscle tone (so moving up and down the stairs can be challenging) and language delays. The physical symptoms can also become the source of more behavioral and emotional symptoms like frequent tantrums, poor self-esteem, social isolation, and mental health struggles like anxiety and depression.
Some of these scenarios are common in all children from time to time, but if you notice a pattern or if these behaviors get in the way of everyday life and functioning, a sensory disorder may be at play. Try our Sensory Processing Disorder test to see if this may be the case for your child.
What Are the Causes of Sensory Integration Disorder?
- Genetic Factors: Traditional doctors often view Sensory Integration Disorders (SID/SPD) as genetic.
- Association with Other Conditions: SID/SPD is frequently seen as part of autism or other neurodevelopmental conditions.
- Environmental Influences: Recent research highlights environmental factors, particularly stress during pregnancy and delivery, impacting the autonomic nervous system and sensory integration function.
- Challenges in Diagnosis: Many doctors struggle to identify the root cause of SID/SPD due to its non-recognition as an official diagnosis.
- Role of Subluxation: SID/SPD often involves subluxation, characterized by misalignment, fixation, and dysautonomia, particularly in the spine, affecting nervous system function and sensory processing.
- Stress and Trauma: Subluxation, contributing to SID/SPD, can be caused and prolonged by stress, trauma, and toxicity, impacting brain and body functions.
Are SID/SPD Symptoms of Autism?
You may have noticed some overlap in SID/SPD symptoms and autism symptoms. While it’s likely that people with autism have some form of SPD, many, if not most, people with SID or SPD don’t have autism. SID and autism have different neurodevelopmental parts, even down to brain matter.
This is part of why there’s such a big movement to have SID and SPD recognized as separate and stand-alone conditions. Pediatric chiropractors, for example, see autism and SID as separate concerns and provide care accordingly.
Care For Sensory Integration Disorders
Because sensory disorders are always related to another disorder or condition, getting the proper care for both the symptoms and the root issues of sensory integration disorders can be discouraging.
Some doctors will employ sensory integration therapy (SI), where children are encouraged to interact with certain sensory stimulation in a safe, low-impact, low-risk environment. These activities are usually designed to be playful or fun for kids while slowly but regularly integrating them with challenging situations. Occupational therapy also helps with SID symptoms by practicing fine motor skills, gross motor skills, and everyday skills such as getting dressed.
A “sensory diet” is another tactic to help kids regulate their sensory responses by having a list of activities they can practice at home and school. This is to encourage children to stay focused during the day so that they can complete their day-to-day functions. For example, a child may need a fidget toy at their desk or the opportunity to go on a short walk every hour.
Many of these solutions are geared towards regulating symptoms and smoothing transitions for sensory kids, not the root cause. While teaching kids how to regulate and expose them to different scenarios can be part of an overall strategy, it’s also best to look and care for the underlying neurological issues. PX Docs and appropriately-trained pediatric chiropractors can provide care for the underlying subluxation and dysautonomia challenges, helping improve the quality of life for SID/SPD patients of all ages.
PX Docs uses a special tool called INSiGHT Subluxation Scanning Technology. In just a 10-15 minute exam, these scans can find, measure, and locate dysautonomia and other elements of subluxation. After the scan, our trained PX Docs can create a customized care plan that may include adjustments that focus on sensory, motor, and other neurological benefits. This personalized plan for your child will target the underlying neurological challenges rather than just the symptoms.
Discover a Simple Solution For Sensory Integration Disorder
If you’re a frustrated parent who is exhausted and concerned because of a sensory disorder and who hasn’t been able to find help from traditional medical doctors, let’s find a lasting solution for your child. Visit our directory to find a pediatric chiropractor near you.