With the rapid and significant rise in birth intervention and birth trauma, we see more and more cases of torticollis (wryneck) in our PX Docs clinic each and every year.
Unfortunately for most parents, traditional medicine has not updated their understanding of what’s causing it and how to best take care of it for some time, leaving most families, like Nathan’s family, with only traditional treatment options like physical therapy that do not get to the root cause of the problem.
Nathan’s torticollis was affecting his quality of life in many different ways. He struggled to hit his milestones, felt stiff, uncomfortable, and locked up most of the time, and suffered from constant ear infections. His mom was desperate to find help and relief for her baby because his occupational therapy wasn’t doing the trick.
While researching one night, Nathan’s rock star momma stumbled upon chiropractic care. Fortunately, there does seem to be a shift happening in this generation of parents who are seeking out Pediatric Chiropractic more often and earlier than ever before! These parents and families are seeing incredible results with a more gentle, effective, long-lasting approach to their child’s torticollis.
What is Torticollis?
Torticollis in an infant is a stiff, stuck, and twisted neck where the child’s head is continually bent to one side, making it difficult to turn and rotate their head and neck in both directions.
While more significant cases are easy to spot by both parents and providers, it’s been our experience that most cases of torticollis are easily overlooked and missed by standard pediatricians. Additionally, too often, parents are told to just “watch and wait” and that they’ll “grow out of it” over time.
What are the Signs and Symptoms of Torticollis?
While torticollis in an older child or adult is most likely going to be accompanied by pain and headaches, for an infant, the signs and symptoms of torticollis look like the following:
- Frequent bouts of crying, irritability, and colic
- Difficulty latching, nursing, and breastfeeding
- Infantile reflux and digestive problems
- Baby’s head tilt to one side with the chin tilted to the other side
- Limited range of motion and ability to move their neck
- Taking the same position, posture, and head tilt every time they are in the car seat or sleeping
- Difficulty sleeping
- Swollen and spastic neck muscle
- Small pea-sized lump in one of the baby’s neck muscles
- Uneven asymmetrical facial features
- Increased likelihood of also having plagiocephaly and gross motor delays
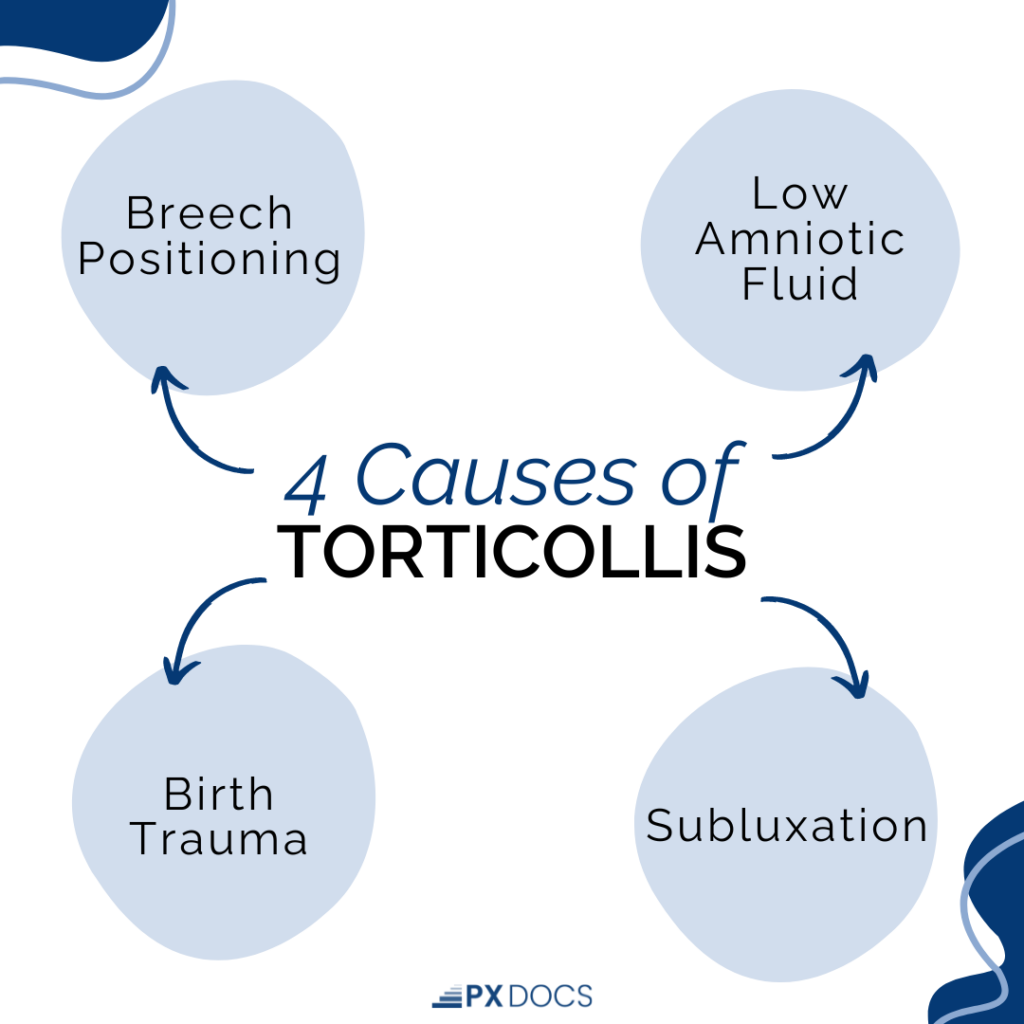
What Causes Torticollis in Infants?
Torticollis is diagnosed medically as congenital if it is caused by abnormal positioning of the fetus while still in the womb, which is more common with things such as breech positioning or lowered amniotic fluid. It will also be diagnosed as congenital torticollis if caused by a genetic condition such as Klippel-Feil syndrome or other genetic disorders affecting the muscular system.
But the most common form of torticollis is acquired, and the most common cause is birth trauma. The amount of physical strain, tension, and pulling placed on a baby’s head and neck during birth interventions such as forceps delivery, vacuum extraction, and C-section is significant and many times leaves the child with a significant subluxation that then contributes to the torticollis.
Subluxation has three (3) main components:
- Misalignment and abnormal positioning of the spinal vertebra
- Fixation and reduced range of motion in the segment and region of the subluxation
- Neurological interference and imbalance caused by reduced amounts of proprioception and increased amounts of nociception
Simply put, the more severe and apparent the torticollis and its related misalignment and fixation, the more severe the subluxation patterns likely are for the child.
Care Options for Torticollis
The first thing we’d encourage parents to do if they’re concerned their child may have torticollis is not just relying on their pediatrician or medical doctor’s exam findings. Of course, pediatricians are trained to perform physical exams in such a way as to spot neuromuscular challenges like torticollis. Still, they don’t have nearly the experience or detailed training in those systems as a Pediatric Chiropractor or Physical Therapist would.
If the pediatrician does spot torticollis for a child, they most likely will make a referral to a PT, who then will show the parents a few positioning and stretching exercises they can do at home to try and help alleviate the torticollis. However, most parents report to us that those stretches and exercises are extremely painful for the child and almost tend to aggravate the condition because it leaves the child in a sustained state of fight-or-flight tension, something known as dysautonomia.
The Pediatric Chiropractic approach to caring for torticollis is so often the one parents feel makes the most sense, and it can be summarized in these three (3) simple and safe steps:
- Find and locate the exact location and severity of the subluxation(s)
- Make safe and gentle neuro-tonal adjustments to relieve the tension and remove the subluxation(s)
- Encourage parents to watch closely for a recurrence of the torticollis around growth spurts, teething, colds, illnesses, or other stressful events the child may experience
Watch this video below to better understand the exam + scan findings from a case of torticollis, and to even watch one of the safe and gentle adjustments we provide!
Additionally, parents routinely report that when they put Pediatric Chiropractic as the foundation and first choice for their child’s torticollis, it then makes all the physical therapy stretches and positioning work easier and far more effective! As PX Docs, we love nothing more than working in conjunction with your child’s therapy team for maximum results!
One of the real keys to caring for torticollis is not just using positioning and range of motion testing as the only clinical criteria for resolving the condition. As Pediatric Chiropractors, we routinely examine and evaluate kids ages 5 and up who had torticollis as an infant, did traditional medical and therapy treatment only, and still have retained torticollis all those years later that is easily found on our exam and INSiGHT Scans neurological evaluation.
You can learn more about the PX Docs Clinical Process and INSiGHT Scans here.
It’s very important for the long-term health and neurodevelopment of your child to get the torticollis fully resolved before releasing them into wellness care, so don’t be surprised if your child’s initial care plan spans a few months of consistent care. If that subluxation and resultant dysautonomia is left in there even at mild to moderate levels, it can begin to contribute to things such as Gross Motor Delays, Fine Motor Challenges, Sensory Integration Disorder, and ADHD later on in life.
Additionally, kids who have unresolved torticollis are going to be more susceptible to ear infections. This is because the muscles in the neck are connected to the muscles in the ear, and when the neck muscles are tight or contracted, they can affect the function of the ear muscles and the Eustachian tube.
The Eustachian tube is a small passageway that connects the middle ear to the back of the throat. Its primary function is to equalize the pressure between the middle ear and the outside environment and to drain fluid from the ear. When the neck muscles are tight or contracted, they can cause the Eustachian tube to become blocked or constricted, leading to a buildup of fluid that is unable to drain in the middle ear. This can create an environment that is conducive to the growth of bacteria, leading to an ear infection.
Torticollis also increases the risk of other respiratory infections developing, such as croup, chronic cough, and even RSV since the torticollis and subluxations limit the body’s ability to drain the fluid from the ears and move mucus and secretions through the respiratory system.
Find Your Local PX Doc Today
In many cases, parents can start to see results and see their child experience relief in just a few visits! Overall it generally takes a few weeks or even a few months (as discussed above) to get full resolution of the torticollis, and your trained and ready PX Doc will sit down with you at what’s called the Report of Findings visit to show and discuss your child’s exact, personalized care plan.
There is no “cookie cutter” approach to torticollis from our PX Docs Network, where each child gets the same stretches and positioning exercises. The examination and scan process is crucial to making sure we find the exact root cause of your child’s challenges and make just the right adjustments to get things taken care of!
One month into Nathan’s care plan, his digestive issues and eczema cleared up. In month two is when his mom saw a huge difference. His mobility improved drastically, he started hitting milestones and said goodbye to ear infections.
To find your local PX Doctor, simply head over to our directory page, plug in your city and state or zip code, and reach out to schedule your consultation and examination today!