As a parent, being jolted awake in the middle of the night by your child’s cries of pain is absolutely heartbreaking. There’s not much you can do for them in the middle of the night, but try to provide comfort while you wait it out.
This is what Luca’s mom faced over and over again each time he had an ear infection. After completing a course of antibiotics, a new bout of ear infection would flare up as soon as the next cold or virus came along. He was on antibiotics back to back for months until the pediatrician suggested going to an ENT for tubes in his ears or some other sort of surgery – but Luca’s mom did not want to go that route.
Moms and dads, that part of Luca’s story might be right where you are now. You absolutely want to stop your child’s recurrent ear infections and continued struggles. Still, you also can’t stand to think of yet another round of antibiotics and do not want to have your child go through surgery if they don’t have to.
Well, that’s the good news we have to share with this article all about Chronic Ear Infections – there is hope, answers, and help that do not involve drugs and surgery!
Chronic Ear Infection Overview
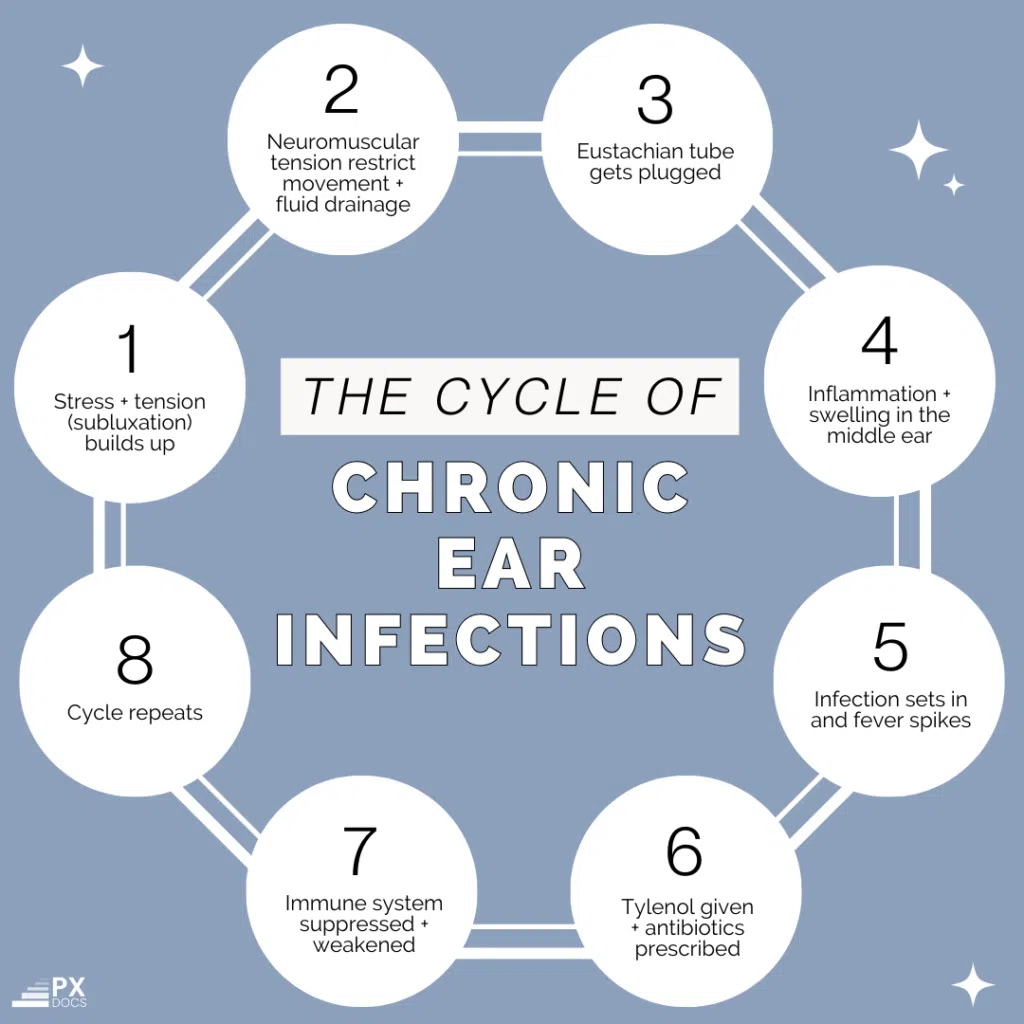
A chronic ear infection is a recurring buildup of fluids, inflammation, and swelling that plugs the eustachian tube in the middle ear, causing repeated pressure and pain.
This condition may often be referred to as chronic otitis media or recurrent ear infections. The number one cause of this condition is poor drainage and “plumbing” of the inner to middle ear through the eustachian tube.
According to the American Academy of Pediatrics, about 60% of children experience at least one ear infection by their first birthday. By the age of three, around 80% of children have had at least one. Respiratory infections such as colds and flu are even more common, and most children will have multiple episodes before age 3.
One study published in the Journal of the American Medical Association (JAMA) found that pediatricians in the United States frequently prescribe antibiotics for ear infections in children, even when the infections are unlikely to be bacterial or severe. The study concluded that antibiotic prescriptions for ear infections could be reduced by implementing more strict adherence to the “Watch and Wait” guidelines.
Another study published in the journal Pediatrics found that the use of antibiotics for children with ear infections decreased when physicians were educated about the guidelines and given tools to follow them. However, the study also found that not all physicians were aware of the guidelines, suggesting that more education and outreach may be needed to improve adherence to the guidelines.
What Causes Chronic Ear Infections?
Most ear infections are caused by the buildup of viruses in the middle ear, while very few are bacterial. This is why, as we’ll address later, antibiotics have long been proven mostly ineffective for both acute and chronic ear infections and have long-term consequences to the child’s health.
Traditional medical treatment for ear infections often misses the mark because targeting the viral infection does not address the root cause of chronic ear infections. The number one issue that causes ear infections in the first place is the buildup of fluid because of poor drainage in the middle ear, eustachian tube, and really the entire ENT, respiratory, and lymphatic system.
Put simply, if the body can’t expel the viruses and bacteria, it becomes chronically congested with them, leading to ongoing inflammation and recurrent, chronic ear infections and other illnesses.
Then, if a child is also experiencing a growth spurt, teething or picks up just a simple common cold from a sibling, daycare, or preschool, the combination of poor drainage and increased fluid buildup can be enough to cause acute and chronic ear infections.
Putting this all together, we find the real culprit with chronic ear infections in kids is poor drainage and plumbing. That whole cascade is often first caused by subluxation in the upper neck, cranial, and upper torso (lungs, lymph nodes) region.
Since so many children experience a tough start to life through birth intervention and birth trauma, and since that physical strain and trauma most commonly affects the cranial and upper neck regions, subluxation in that area for so many kids is the primary culprit behind chronic ear infections.
Since pediatricians and ENTs are not trained to find and detect subluxation and neuromuscular interference, and since they only really know about drugs and surgery, this is why, still today, millions of kids end up going through countless rounds of antibiotics and ear tube surgeries unnecessarily.
Symptoms and Signs of a Chronic Ear Infection
A chronic ear infection occurs when all the traditional signs of an ear infection listed below are present for an ongoing duration of 3 months or more.
Signs of these ear infections include:
- Ear pain and discomfort that feels like pressure in the ear
- Usually a low grade fever
- Fussiness and crying
- Pus-like drainage from the ear
- Hearing loss
- Trouble sleeping
Who’s at a Higher Risk of Getting Chronic Ear Infections?
Once again, the traditional medical system will focus on the more outdated and obvious explanations for the high risk of chronic ear infections. They’ll most commonly discuss things such as children having shorter or more narrow eustachian tubes and having parents or care providers who smoke around the child often.
But in our work as PX Docs, digging way deeper into finding the true cause of children’s health challenges, we repeatedly find the following correlations and case history findings increase the risk of a child developing chronic ear infections:
- A stressful, emotionally challenging pregnancy for the mother
- Birth interventions and trauma, such as forceps, vacuum extraction, induction, and C-section delivery
- Health challenges as an infant, such as colic, reflux, and constipation
- Early exposure to antibiotics and steroid-based medications
- An early diet high in dairy, grains, gluten, etc.
Each of those early stressors increases the tension and stress on the nervous system, leaving it stuck in a more sustained sympathetic fight-or-flight response. That sustained sympathetic and subluxation then increases the tone and tension on all the soft tissues and muscles, including the Tensor Veli Palatini muscle we mentioned above, which gets too tight and wound up and stops proper drainage of the eustachian tube.
Additionally, sustained sympathetic tone creates a condition called dysautonomia, which leaves the body in a more inflammatory state and weakens the immune response.
Treatment for Chronic Ear Infections
If you’re reading this article, you are likely searching for treatment options that go beyond traditional antibiotics, medications, and surgery. If so, it’s essential to first explain to all parents that natural health and neurologically-focused pediatric chiropractors within our PX Docs Network do not seek to treat or cure chronic ear infections at all.
Instead, we take the approach of taking care of the root cause(s) of the chronic ear infections and working to restore proper balance and function to the nervous system, immune systems, and nerves and muscles that are involved in keeping the inner and middle ear healthy, draining, and functioning just right.
The first thing parents report when getting their children struggling with chronic ear infections adjusted and under chiropractic care is that they can finally drain and clear the fluid easily and sleep much better at night. This improved drainage and sleep help the body fight off the infection and clear things out much faster, meaning the body itself is doing the healing, just as it’s designed to do!
In addition to these incredible chiropractic adjustments, there are many natural remedies parents and providers can use to help with chronic ear infections. You can find all those resources here on our site!
Prevention for Chronic Ear Infections
Without a doubt, preventing acute and chronic ear infections goes all the way back to the foundations of keeping the nervous system, immune system, and respiratory system balanced and functioning at their best. If there is too much stress, subluxation, and inflammation in the body, the child is susceptible to any and all illnesses. Young kids will be most prone to chronic ear infections since the first year or two of life, they are not moving (walking, running) as much on their own, and also go through so many rounds of teething and the natural congestion that causes.
Additionally, focusing on keeping the nerves and muscles of the upper neck, cranial system, and upper thoracic area free and clear of subluxation and interference is very important in helping prevent chronic ear infections.
After 15 years of clinical practice, we have found again and again that children receiving regular chiropractic care and living a clean, natural lifestyle have by far the lowest incidence of acute and chronic ear infections, and then in turn, get through illnesses and ear infections must faster, almost always achieving resolution without the use of antibiotics.
While a few studies, such as this one, show the results of chiropractic care for ear infections, many larger-scale studies need to be done going forward.
Especially when we consider the known dangers and side effects associated with antibiotics, medications, and surgery, parents today are definitely looking to natural, drug-free options like chiropractic care and natural remedies first.
One final thing to remember is that each time your child gets through an infection or illness naturally on their own, perhaps with natural defense-boosting options like chiropractic, they come out stronger and more resilient on the other side. So, while it absolutely stinks to watch our children struggle with illnesses and infections, knowing they will get stronger on the other side helps lessen some of our stress and anxiety as parents.
Next Steps for Parents of Kids with Chronic Ear Infections
Honestly, parents, we can simplify this down to two simple steps for you to take right away:
First, be sure to read the Natural Remedies for Ear Infections article and download the Raising Healthy Kids Naturally Playbook. That will help you with all sorts of action steps you can take at home, from the right diet changes to supplements and herbs that can help boost your child’s natural defenses!
Second, after reading this article, you think that subluxation may be playing a role in your child’s chronic ear infections, so get over to our PX Docs Directory and book an appointment with your local Pediatric Chiropractor today!
That was Luca’s family’s most impactful move, and you can read his full story of natural health and healing from chronic ear infections here. For Luca, it was not only that he was able to finally stop suffering from the pain and sleep disturbances the ear infections caused, but he finally could stop taking those dangerous antibiotics and also started to physically grow again since his body had been so tired and worn out from all the stress and struggle.
For more information on how Pediatric Chiropractic and our PX Docs Clinical Process works, watch the explanatory video above from Dr. Tony. He’ll show you what to look for in the case history, how we use an incredible piece of technology called the INSiGHT Scans to find and detect subluxation, and explain exactly how the adjustment works!