Living with Postural Orthostatic Tachycardia Syndrome (POTS) can feel like an uphill battle, and like you’re living each day on a roller coaster. Even on the good days, you’re worried that another spell of trouble is just around the corner with the slightest change in how you move, your stress levels, or even uncontrollable things like the weather.
Imagine your teenage daughter struggling to get out of bed each morning, feeling dizzy and lightheaded every time they stand up. They cannot concentrate in school, participate in sports, or enjoy social activities with friends. Despite numerous doctor visits and tests, you’re left without answers, watching helplessly as your once vibrant child’s life is put on hold.
This is the reality for many of the estimated one to three million Americans living with POTS, a complex condition of the autonomic nervous system that causes an abnormally rapid heart rate upon standing. POTS characteristics can range from mild to debilitating, significantly impacting patients’ quality of life and daily functioning.
Unfortunately, POTS is often misunderstood and misdiagnosed, leaving patients and their families feeling frustrated and alone. Conventional medication approaches may provide relief, but they often fail to address the root cause of this mysterious condition.
But what if there was a missing piece to the POTS puzzle? A growing body of research suggests that the key to understanding and caring for children with POTS may lie in the complex relationship between the brain, nervous system, and the rest of the body.
By taking a deeper, more foundational look at the neurophysiology behind POTS, we help our patients uncover a layer of root cause dysfunction that is not often found elsewhere in healthcare. In this article, we’ll dive deep into the role of things like subluxation, nervous system dysregulation, and even proprioception – all terms that anyone suffering from POTS will want to become fully familiar with in order to get the best results possible from their care program.
Understanding POTS
Postural Orthostatic Tachycardia Syndrome (POTS) is a dysfunction characterized by an abnormal increase in heart rate upon standing. The current diagnostic criteria for POTS is a heart rate increase of 30 beats per minute (bpm) or more within the first 10 minutes of standing, in the absence of orthostatic hypotension. For children and adolescents, the criterion is a 40 bpm or more increase.
POTS patients may experience a wide range of characteristics, including:
- Dizziness or lightheadedness upon standing
- Fatigue and weakness
- Headaches
- Brain fog and difficulty concentrating
- Heart palpitations
- Tremors or shaking
- Nausea and gastrointestinal issues
- Heat intolerance
- Sleep disturbances
These symptoms can vary in severity from patient to patient, but for many, they can be debilitating. Simple tasks like getting out of bed, taking a shower, or preparing a meal can become daunting challenges. Students with POTS may struggle to attend school regularly or keep up with their coursework. Adults may find it difficult to maintain employment or care for their families.
The impact of POTS extends beyond physical symptoms. Many patients experience anxiety, depression, and social isolation due to their condition. Perhaps the worst part is the nonstop feeling of exhaustion and depletion. The unpredictable nature of signs can make it challenging to plan activities or commitments, resulting in feelings of frustration and disappointment.
POTS has been known by various names throughout history, including DaCosta’s Syndrome, Soldier’s Heart, and Chronic Orthostatic Intolerance. In 1993, a team of researchers led by Dr. Philip Low of the Mayo Clinic coined the term “Postural Orthostatic Tachycardia Syndrome.”
Since then, researchers have identified several subtypes of POTS, including:
- Neuropathic POTS, associated with damage to the peripheral nervous system
- Hyperadrenergic POTS, characterized by elevated levels of norepinephrine
- Hypovolemic POTS, related to low blood volume
- Autoimmune POTS, linked to autoimmune conditions like Sjogren’s syndrome or Lupus
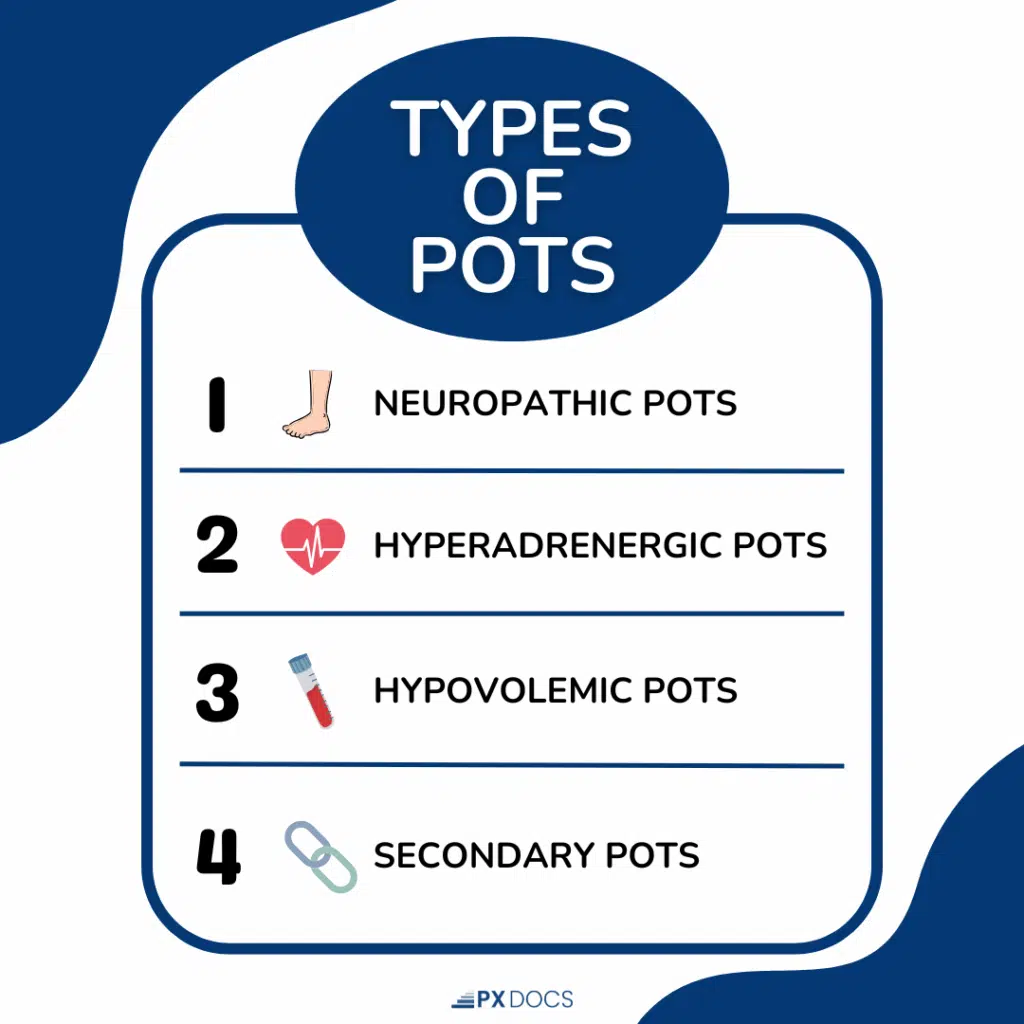
While there is no specific subtype for autoimmune POTS, research shows that approximately 20% of patients have an identifiable autoimmune condition. Understanding the different presentations of POTS is crucial for providing personalized and effective care. By recognizing the complexity and variability of this condition, we can move towards a more comprehensive approach to an individual care plan, and not just rely on conventional approaches like medications and moving more slowly when shifting positions
Misconceptions about POTS
One of the most pervasive and harmful misconceptions about POTS is that it is caused by anxiety. This belief stems from the fact that some of the physical traits of POTS, such as tachycardia and palpitations, can mimic those of anxiety conditions. However, research has shown that POTS is not a psychological condition, but rather a physiological condition rooted in nervous system dysregulation.
Studies have found that POTS patients are no more likely to experience anxiety than the general population. Many POTS patients develop anxiety as a result of their condition, not the other way around. The constant stress of managing signs and navigating daily life with a chronic illness can take a significant toll on mental health.
Another misconception is that POTS disease can be effectively managed through conventional medical care alone. While medications like beta-blockers and fludrocortisone can help alleviate some symptoms, they often fail to address the root cause of the condition, and like all medications – may make things worse over time, not better. Patients may find themselves stuck in a management cycle, never fully regaining their quality of life.
The limitations of conventional approaches highlight the need for a paradigm shift in our understanding and care of POTS. Rather than viewing it as an isolated condition, we must recognize that POTS is a manifestation of a deeper imbalance within the body’s regulatory systems.
This new perspective should take into account:
- The complex interplay between the nervous system, cardiovascular system, and other body systems
- The role that core neurosensory functions like proprioception and sensorimotor input play, along with the neurospinal system, brainstem, and cerebellum
- The role of factors like cervical instability, genetic predisposition, and environmental triggers in the development of POTS
- The potential for Neurologically-Focused interventions, such as chiropractic care, to restore balance and function to the autonomic nervous system
By embracing a more integrative approach to POTS, we can move beyond management and work towards true healing for patients. This paradigm shift requires a willingness to challenge long-held assumptions and explore new avenues of research and care plans.
The Autonomic Nervous System and POTS
To understand the underlying mechanisms of POTS, it’s essential to have a basic understanding of the autonomic nervous system (ANS) and its role in maintaining homeostasis within the body. The ANS is responsible for regulating involuntary functions such as heart rate, blood pressure, digestion, and temperature control.
The ANS consists of two main branches:
- The sympathetic nervous system (SNS), which activates the “fight or flight” response during times of stress, increasing heart rate and blood pressure.
- The parasympathetic nervous system (PNS), which promotes “rest, regulation, and digestive” functions, slowing heart rate and promoting relaxation.
In a healthy individual, the SNS and PNS work together to maintain balance and adapt to changing conditions. However, in people with POTS disease, this delicate balance is disrupted, leading to a condition called dysautonomia.
Dysautonomia refers to a dysfunction of the ANS that results in an overactivation of the SNS and an underactivation of the PNS. This imbalance can cause a wide range of symptoms, including tachycardia, dizziness, and blood pooling in the extremities. Sympathetic overdrive is a hallmark sign and trigger of POTS, as is parasympathetic fatigue and exhaustion.
Think of the ANS as a complex system of checks and balances, with the SNS acting as the gas pedal and the PNS as the brake. In POTS patients, it’s like the gas pedal is stuck, revving the engine (heart rate) without the brake (PNS) to counteract it. This leads to the hallmark trait of POTS: an abnormal increase in heart rate upon standing.
But the effects of dysautonomia extend beyond just heart rate. The ANS also regulates blood vessel constriction, which helps maintain adequate blood flow to the brain when we stand up. In POTS patients, this mechanism is impaired, leading to dizziness, lightheadedness, and even fainting.
Furthermore, dysautonomia can affect other bodily functions regulated by the ANS, such as:
- Digestion, leading to nausea, bloating, and other gastrointestinal symptoms
- Temperature regulation, causing heat intolerance or excessive sweating
- Sleep, contributing to insomnia or sleep disturbances
Lastly, and just as importantly, subluxation disrupts and distorts proper proprioceptive and mechanoreceptive (position sense) sensory input into the spinal cord, brainstem, and cerebellum. Because subluxation does not show up on any conventional or even integrative medical exams, it’s by far the most overlooked aspect of POTS, even in holistic circles.
By understanding the central role of the ANS, subluxation, and dysautonomia in POTS, we can begin to develop targeted interventions that aim to restore balance and improve patient outcomes. We’ll look into the various factors that can contribute to dysautonomia and how a Neurologically-Focused Chiropractic Care approach may hold the key to effective POTS management.
The “Perfect Storm”: Factors Contributing to POTS
The development of POTS disease is often the result of what we call the “Perfect Storm” of factors that converge to create a state of autonomic dysfunction. While the exact causes of POTS vary from person to person, research has identified several common contributors:
- Genetic predisposition: For concerned parents wondering, “Is pots genetic?” Studies suggest that there may be a genetic component to POTS, with 14% of patients having a family member with the condition.
- Viral infections: Many POTS patients report a sudden onset of signs following a viral illness, such as mononucleosis or the flu.
- Chronic stress: Prolonged exposure to physical or emotional stress can take a toll on the autonomic nervous system, leading to dysregulation over time.
- Hormonal changes: POTS is more common in women, particularly during adolescence and young adulthood, suggesting a possible link to hormonal fluctuations.
- Autoimmune Conditions: Some cases of POTS may be associated with autoimmune conditions like Sjogren’s syndrome or lupus.
- Physical deconditioning: Prolonged bed rest or inactivity due to illness or injury can lead to deconditioning of the cardiovascular and autonomic systems.
These factors can interact and compound over time, creating a snowball effect that ultimately leads to the development of POTS. Understanding the complex interplay of these contributors is crucial for developing targeted, individualized care plans that address the root causes of the condition.
The Neurological Roots of POTS
While POTS is often characterized as a condition of the autonomic nervous system, recent research suggests that its roots may lie in the central nervous system, particularly in the brainstem and spinal cord.
The brainstem, which houses the regulatory centers for heart rate, blood pressure, and other autonomic functions, has been implicated in the development of POTS. Studies using advanced imaging techniques have found structural and functional abnormalities in the brainstem of POTS patients, including:
Reduced volume of gray matter in the medulla oblongata
- Altered connectivity between the brainstem and other brain regions involved in autonomic regulation
- Impaired signaling between the brainstem and the peripheral nervous system
In addition to brainstem dysfunction, many POTS patients exhibit signs of cervical instability or misalignment, which can lead to a condition called cervical dysautonomia. When the upper cervical spine is misaligned and subluxated, it can cause interference within the intricate network of delicate nerves and blood vessels that pass through the neck and brainstem, disrupting communication between the brain and the autonomic nervous system.
This combination of brainstem abnormalities and cervical instability creates a “double whammy” effect, further exacerbating autonomic dysfunction and contributing to the wide range of symptoms experienced by POTS patients. Often, the cervical instability in the upper neck and brainstem regions comes from long-standing tension and restriction of the nerves and muscles in the lower neck, traps, and upper to mid back region. If a patient struggles with chronic pain and tension in these areas, it’s strongly correlated with the neurophysiological triggers of POTS and other related neurological conditions.
Neurologically-Focused Chiropractic Care for POTS
Neurologically-Focused Chiropractic Care is a specialized approach that aims to restore balance and function to the nervous system by addressing subluxation and dysregulation with a safe, gentle, drug-free approach. For POTS patients, this approach can be particularly effective in reducing daily struggles and improving quality of life.
The first step in Neurologically-Focused Chiropractic Care is a comprehensive evaluation using advanced tools, such as:
- INSiGHT Scanning: This non-invasive technology measures the electrical activity of the nervous system, identifying areas of dysfunction or imbalance.
- Precision Radiographs: If necessary, high-resolution X-rays allow chiropractors to visualize the alignment of the spine and identify any areas of instability or misalignment.
- Autonomic Response Testing: This technique enables chiropractors to assess the function of the autonomic nervous system and pinpoint specific areas of dysfunction.
By addressing the neurological roots of POTS, chiropractic care can help patients achieve lasting relief from symptoms and improve their overall functioning. In fact, studies support the effectiveness of chiropractic interventions for POTS and other autonomic conditions.
Lifestyle Modifications and Other Care Options
In addition to Neurologically-Focused Chiropractic Care, there are several lifestyle modifications and complementary care that can help POTS patients manage their symptoms and improve their quality of life:
- Hydration: Drinking plenty of fluids, particularly water and electrolyte-rich beverages, can help increase blood volume and reduce signs of dizziness and lightheadedness.
- Salt and mineral intake: Increasing salt and mineral consumption, under the guidance of a healthcare provider, can help retain fluids and improve blood pressure regulation.
- Compression garments: Wearing compression stockings or abdominal binders can help reduce blood pooling in the extremities and improve circulation.
- Recumbent exercise: Low-impact exercises performed in a reclined or seated position, such as swimming, recumbent biking, or rowing, can help improve cardiovascular conditioning without exacerbating symptoms.
- Nutrition: Eating a balanced diet rich in whole foods and low in processed, high-sugar items can help support overall health and reduce inflammation.
- Stress management: Practices like deep breathing, meditation, and yoga can help reduce stress and promote relaxation, which is crucial for regulating the autonomic nervous system.
The most effective care plans for POTS often involve a combination of these lifestyle modifications and complementary therapies, with Neurologically-Focused Chiropractic Care and autonomic regulation serving as the foundation..
Prognosis and Long-Term Management
The prognosis for POTS patients varies widely, depending on the underlying causes, the severity of symptoms, and the effectiveness of care. While there is no known cure for POTS, many patients experience significant improvement with proper management and care.
Long-term management of POTS typically involves a combination of ongoing chiropractic care, lifestyle modifications, and self-management strategies. Regular chiropractic adjustments can help maintain proper alignment and function of the nervous system, while lifestyle factors like hydration, nutrition, and exercise can support overall health and reduce the frequency and intensity of characteristics.
Perhaps most importantly, POTS patients need ongoing support and validation from their healthcare providers, family, and friends. Living with a chronic, often invisible illness can be isolating and emotionally challenging, and having a strong support system can make a significant difference in a patient’s ability to cope with their condition and maintain a positive outlook.
Empowering Patients Through Knowledge and Care
Living with POTS can feel like a constant battle, but it’s one that patients don’t have to fight alone. By understanding the neurological roots of this complex condition and seeking out specialized, multidisciplinary care, patients can take control of their health and work towards achieving lasting relief from their POTS symptoms.
At the heart of this approach is a commitment to patient education and empowerment. By providing accurate, up-to-date information about the underlying causes of POTS and the various care plans available, healthcare providers can help patients make informed decisions about their care and advocate for their own needs.
Neurologically-Focused Chiropractic Care is an important piece of this puzzle. By addressing the root causes of autonomic dysfunction and restoring balance to the nervous system, chiropractors can help POTS patients achieve significant improvements in their symptoms and quality of life.
If you or a loved one is struggling with POTS, know that there is hope. Take the first step towards healing by visiting the PX Docs directory and scheduling a consultation with a neurologically-focused chiropractor near you. With the right knowledge, care, and support, you can unlock your body’s innate potential for healing and regain control of your health and your life.