Living with POTS Syndrome can be extremely challenging for both the individual diagnosed and struggling with it and for their parents and family members looking to support and help them in any way possible. Like many other conditions affecting teenage and young adult females, POTS can have a seemingly sudden onset and take a healthy and active person and greatly wreck their quality of life rather quickly.
That is what happened to our patient Tommi. She went from being a wildly active and athletic high school student to barely being able to get through the basic functions of everyday life. Here’s what her mom wrote on the intake paperwork, truly describing the many struggles patients with POTS Syndrome experience each day.
The symptoms that she has been experiencing are associated with her POTS diagnosis, which has completely derailed her 17-year-old life. The massive fatigue that she experiences keeps her in bed all day long, and the migraine headaches and brain fog that have made it impossible for her to do any schoolwork for the last 4 weeks. She has also been experiencing each of the following to varying degrees: lightheadedness and dizziness upon standing (sometimes upon sitting upright); tachycardia; low blood pressure; high heart rate; nausea and stomach pain; chest pain; neck pain; blurry vision; getting really hot and/or really cold; insomnia; anxiety and depression. The brain fog is so very troubling to me; it is almost as if she cannot form the thoughts needed to bring her from point A to point B to point C. She was an A-B student before this all started, and now just trying to decide which homework subject to work on totally shuts her down.
While most medical doctors still primarily blame genetics (like usual) or a recent injury or viral infection, when we dive deep into the case history of our patients like Tommi, we find quite a history of significant stressors that stack up and lead to these challenges within the Autonomic Nervous System and Vagus Nerve, two key things you’ll learn all about in this article.
This article will help you not just find those true root causes of POTS Syndrome but also help patients and parents find drug-free options and action steps they can take to restore balance to the Autonomic Nervous System and get their quality of life back!
What is POTS Syndrome?
POTS Syndrome, also known as Postural Orthostatic Tachycardia Syndrome, is a disorder that affects the Autonomic Nervous System, causing an abnormal increase in heart rate and many other debilitating symptoms upon assuming an upright posture.
POTS is not a single condition but rather a group of disorders characterized by similar symptoms, much like Dysautonomia and Vagus Nerve Disorders. In fact, you’ll see throughout this article that those two conditions are the likely underlying causes of POTS Syndrome more so than anything else.
It’s also important for patients and parents to know that there are a few different subtypes of POTS Syndrome:
Neuropathic POTS
Neuropathic POTS, a specific subtype of POTS syndrome, is closely associated with dysfunction in the autonomic nerves that regulate heart rate and blood vessel constriction. One crucial nerve involved in autonomic control is the Vagus Nerve.
When the Vagus Nerve experiences damage or dysfunction, known as subluxation, it can disrupt the delicate balance of the autonomic nervous system, leading to symptoms commonly seen in POTS, such as tachycardia, lightheadedness, and postural blood pressure fluctuations.
The Vagus Nerve plays a vital role in regulating various bodily functions, including heart rate, digestion, and blood pressure. Dysfunction (subluxation) of the vagus nerve can disrupt the communication between the brain and the body, leading to dysautonomia — a condition characterized by an impaired autonomic nervous system.
Dysautonomia can manifest in different ways, such as orthostatic intolerance (inability to tolerate an upright position), gastrointestinal issues, temperature regulation problems, and sleep disturbances, as well as behavioral or emotional dysregulation. Understanding the connection between Neuropathic POTS and Vagus Nerve Dysfunction is essential in developing targeted care options that address the underlying nerve dysfunction (subluxation), promote symptom relief for individuals with POTS syndrome, and help restore their quality of life in a major way!
Hyperadrenergic POTS
Hyperadrenergic POTS is another variant, typically associated with an excess release of norepinephrine, a stress hormone. This type of POTS often manifests with symptoms such as palpitations, anxiety, and elevated blood pressure.
Since the adrenal glands primarily respond to stimulation and activation of the Sympathetic Nervous System, this subtype of POTS Syndrome can often be traced back to the Neuropathic Type and Dysautonomia.
Hypovolemic POTS
Hypovolemic POTS occurs when there is a decrease in blood volume within the body. This can result from factors such as dehydration, blood loss, or certain medical conditions. Symptoms may include fainting, rapid pulse, and difficulty concentrating.
Secondary POTS
Secondary POTS develops as a result of another underlying condition, such as Ehlers-Danlos syndrome or autoimmune diseases. Identifying and treating the primary condition is crucial in managing secondary POTS effectively.
Symptoms of POTS Syndrome
The symptoms experienced by individuals with POTS syndrome can vary, but some common manifestations include:
- Dizziness
- Fainting
- Forgetfulness + brain fog
- Heart palpitations + tachycardia
- Anxiety
- Exhaustion
- Shortness of breath
- Headaches
- Bloating
- Nausea
- Chest pain
These symptoms can significantly impact daily life, leading to reduced mobility, difficulty in performing tasks, and emotional distress.
What are the Causes of POTS Syndrome?
Current medical research has revealed certain factors associated with the development of POTS Syndrome, noting that it can often begin following events such as pregnancy, major surgery, trauma, or a viral illness.
Diving deeper, for the majority of the patients I’ve seen diagnosed with POTS, there was even more “trauma before the trauma” that traditional doctors did not quite understand and factor in.
Since POTS Syndrome is generally not experienced and diagnosed until the teenage or young adult years, most doctors just don’t go back far enough to the patient’s case history to really put together all the clues and start to see what we call “The Perfect Storm” pathway or pattern emerge.
Here are a few of the things we see again and again in the case history of our POTS Syndrome patients that we feel strongly need to be investigated and researched further for their connections to POTS, Dysautonomia, and so much more. They are:
- Birth interventions + trauma (forceps, vacuum, c-section, induction, etc.)
- Infantile colic, reflux, and constipation
- Recurrent ear infections, respiratory infections, allergies, etc.
- Frequent use of antibiotics and corticosteroid medications
While each of those significant stressors may have been experienced way early in life, they lead to disruption and dysfunction within the nervous system and overall health, development, and resiliency later in life. This leaves Perfect Storm kids more susceptible to all sorts of neurological challenges later on in life, including POTS Syndrome and Dysautonomia.
Medical Care Options for POTS Syndrome:
The medications used to treat POTS Syndrome are those that target the symptoms of the condition, not its root cause, just like the majority of medical care and medications.
One commonly prescribed medication for POTS is fludrocortisone, a mineralocorticoid that helps increase blood volume and regulate blood pressure. Beta-blockers, such as propranolol or metoprolol, are also commonly used to control heart rate and reduce palpitations. Additionally, medications that target specific symptoms, such as anti-nausea drugs for gastrointestinal issues or pain medications for headaches or chest pain, may be prescribed when necessary.
Nearly every single patient and parent reports to us that the more medications they are prescribed, the worse they feel and function. One medication may treat one symptom but then create one or more other symptoms as a result, and the cycle continues. Most patients report lowered quality of life with more medication, not better.
Drug-Free Care Options for POTS Syndrome
Fortunately, there are various care options available for individuals facing POTS syndrome, and most patients start with these first:
- Exercise + Postural Training: Engaging in regular, low-impact exercise can help improve cardiovascular function and reduce symptoms, with things like yoga and more easy-going exercises being the best place to start.
- Diet and Nutrition: A balanced diet that includes adequate hydration is crucial for managing POTS symptoms. Incorporating foods rich in vitamins, minerals, and electrolytes can promote overall wellness.
- Compression: Wearing compression garments, such as compression stockings, can aid in improving blood flow and minimizing orthostatic intolerance
While each of those three (3) drug-free care options are wonderful things we wholeheartedly support as Neurologically-Focused Family Chiropractors, just like medications, most patients and parents report that despite trying each of these, the struggles with POTS Syndrome still persist.
This means one thing – something is still missing.
Our clinical experience continually finds that the one thing missing is truly the role that Subluxation, Dysautonomia, and Vagus Nerve Dysfunction play in the development of POTS Syndrome and its symptoms. Therefore, consulting with a trained Neurologically-Focused Pediatric Chiropractor from our incredible PX Docs Network may be the final missing link you’ve been searching for this whole time!
The first thing we do is dive deep into your specific case history, not just looking for the common and obvious things like recent viral infections or traumas but going back all the way to the early life stressors and neurological development overall. It’s important we have a full and complete understanding of what’s going on with the Autonomic Nervous System, and we first assess just that through in-depth case history and consultation.
Then from there comes the most important test any POTS patient could ever have, our Neurological INSiGHT Scans, which include the following three (3) exams that are instrumental (pun intended) in getting to the root cause of POTS Syndrome and Dysautonomia:
- NeuroThermal Scan: measures for imbalances and disruptions on autonomic regulation of the tissues, organs, and glands (i.e. thyroid, adrenals, digestion, etc.).
- NeuroSpinal EMG Scan: detects and measures areas or regions of excessive neuromuscular tension, asymmetry, and imbalance, as well as helps pick up on neurological fatigue and exhaustion.
- Heart Rate Variability (HRV) Scan: the ultimate “stress test” that measures the interbeat intervals with the patient’s heartbeat to determine the balance between the sympathetic (fight-or-flight) and parasympathetic (rest-and-digest) branches of the ANS.
HRV, Chiropractic, and POTS Syndrome
We are very confident that the future of POTS Syndrome and Dysautonomia care will truly center around Heart Rate Variability (HRV) testing and monitoring and Neurologically-Focused Chiropractic Care. Our PX Docs are truly on the leading edge of this field, using HRV in the following ways with our POTS, Dysautonomia, and other complex neurological cases.
For patients with POTS syndrome, an HRV scan can be beneficial in several ways:
- Assessing ANS Function: POTS is primarily characterized by dysautonomia involving abnormal regulation of the ANS. HRV analysis allows healthcare providers to assess the autonomic control of heart rate and identify any imbalances or dysfunction present in the sympathetic and parasympathetic systems. This information helps in understanding the underlying mechanisms contributing to POTS symptoms, as well as determining the severity of the patient’s current condition and status.
- Objective Diagnosis: HRV analysis can aid in diagnosing POTS syndrome by providing objective measurements of autonomic function. It helps differentiate POTS from other conditions and provides supportive evidence when combined with clinical evaluations and other diagnostic tests.
- Care Plan Monitoring: HRV scans can be used to track the effectiveness of care programs and interventions for POTS, specifically progress and improvements made by Neurologically-Focused Chiropractic Adjustments. Our PX Docs measure HRV on very consistent intervals throughout the Clinical Care Program. They are able to use it to best determine adjustment frequency, technique choice and effectiveness, and more.
In summary, HRV and Neurologically-Focused Chiropractic Care are often life-transforming for patients with POTS Syndrome, helping them get right to the root cause of their struggles and accurately measure care program effectiveness and progress every step of the way.
Make sure that no matter what else you put in play to help improve your (or your child’s) POTS Syndrome, that Neurologically-Focused Chiropractic Care and HRV are the absolute foundation of it.
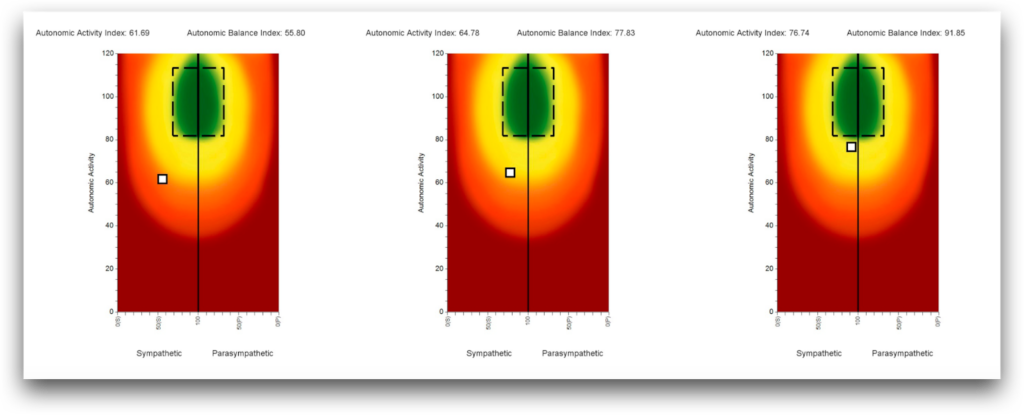
Above is an example of an HRV Scan Series in a POTS Syndrome and Dysautonomia patient, with the first scan on the left showing sympathetic dominance and overall neurological exhaustion as the white dot is shown to the far left and low on the HRV graph.
Then from there, you can see the progression and objective improvement in Autonomic Nervous System function as they went through a series of Neurologically-Focused Chiropractic Adjustments done as part of the Neurological Intensive Program we offer at our practice, PWC Chiropractic outside of Chicago.
As care progressed and neurological function was restored, the patient first experienced improvements in sleep, digestive function, and posture. Then from there started to notice improvements such as a lowered rate and less tachycardia, more energy, and improved mood and mental health, as well as decreased anxiety and emotional dysregulation symptoms.
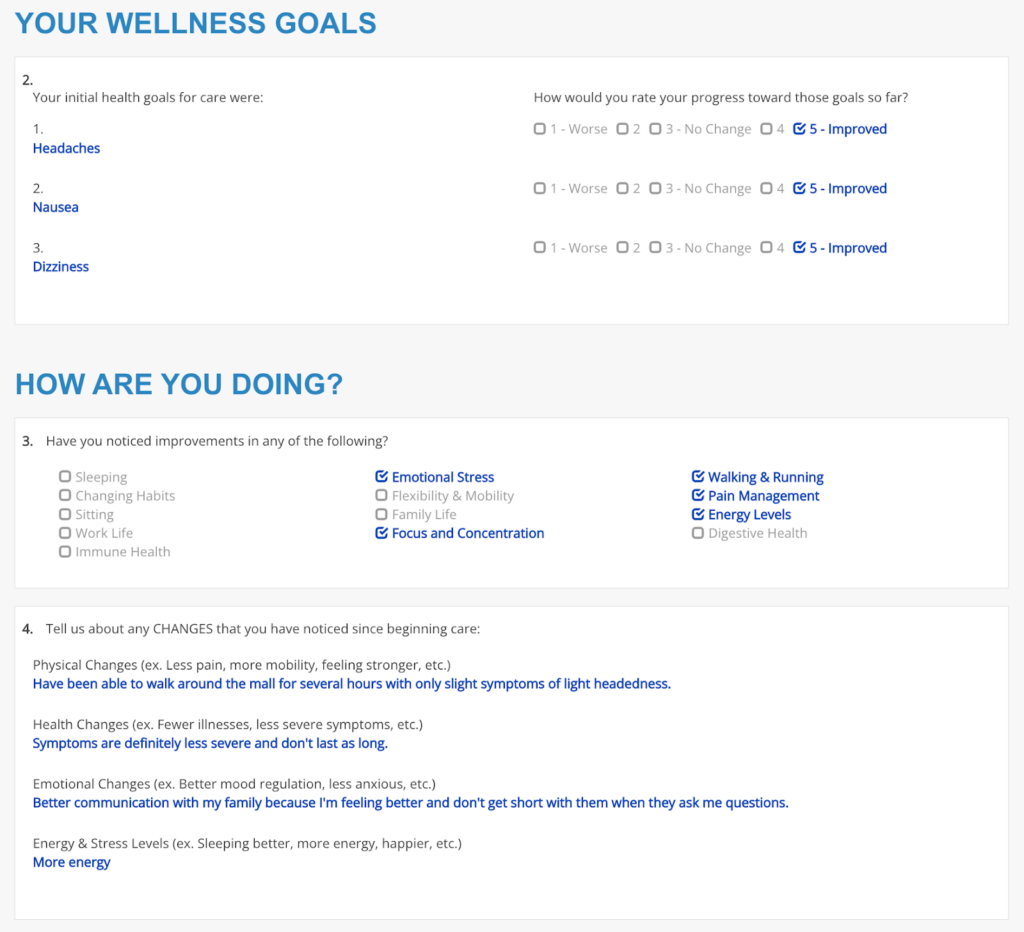
Remember Tommi, whose struggles with POTS Syndrome we mentioned at the start of the article? Here’s how she was doing just 2 weeks into our Intensive Care Program!
Learn More and Find Your Local PX Doctor Today
If you’ve got more questions as to exactly how Neurologically-Focused Chiropractic Care works and what the process is to get started, please check out this page for step-by-step explanations and instructions on just that.
Then when you’re ready to get started and book your Consultation + INSiGHT Scans (HRV) appointment, simply visit our directory here and plug in your city, state, and zip code! We can’t wait to hear your story of overcoming POTS and getting back to the full, vibrant life you deserve!
Every Patient Counts,
Dr. Tony Ebel + The PX Docs Network
PS. If your child’s POTS Syndrome struggles are severe and it seems like you’ve exhausted all options for this tough neurological condition, please consider our 2-Week Perfect Storm Neurological Intensive Program. You can find more information about that incredible program here.





