You did everything right – sessions, strategies, and follow-through. Your child could show progress in therapy, yet daily life remained overwhelming. That gap isn’t a failure of effort or love. It’s what happens when we try to change behavior without first helping the nervous system feel safe and regulated.
While we feel it is a much better first step than doling out dangerous ADHD prescription medications, it’s still common to hear that children don’t respond adequately to Cognitive Behavioral Therapy (CBT) or Applied Behavior Analysis (ABA).
Parents put a lot of effort and time into these strategies, but still end up feeling frustrated and right back where they started.
Behavioral symptoms aren’t always behavioral problems.
Sometimes the challenge isn’t behavioral at all – it’s neurological. When a child’s nervous system is overwhelmed or dysregulated, traditional behavioral strategies can fall short. What’s often labeled as “care-resistant” is really a nervous system that needs support before it can respond.
Why Behavioral Therapy Doesn’t Work for Everyone
Behavioral therapy works for many people. CBT and ABA have decades of research showing effectiveness when a child’s nervous system can access their learning centers.
But the nervous system has veto power over everything.
When your child’s body thinks it’s in danger – even when it’s not – rational thinking, impulse control, and emotional regulation go offline. Research on stress shows that when the Sympathetic Nervous System activates, blood flow shifts away from the prefrontal cortex (your child’s “thinking brain”) toward the brain stem and limbic system that handle survival.
Behavioral therapy teaches better skills. That’s valuable. But if the gas pedal is stuck down and the brake pedal doesn’t work? No amount of training will unstick those pedals.
Here’s the reality: your child can learn skills in the therapy room, but those skills disappear at home. Why? The therapy room is controlled – lower sensory input, predictable routine, one-on-one attention. In that setting, your child’s nervous system can sometimes stay regulated.
But real life isn’t a therapy room. When your child encounters real-world triggers, their nervous system shifts into survival mode. The body prioritizes survival over learning. The amygdala takes over, the prefrontal cortex goes dim, and all those practiced skills are locked behind a door your child can’t access.
This is physiology. You can’t think your way out of a dysregulated nervous system.
When the foundation of nervous system regulation is missing, behavioral therapy becomes just another demand your child can’t meet. The therapist sees “noncompliance.” You see your child struggling. What you’re both seeing is a child whose body won’t let them access the tools they’ve been taught because their nervous system is stuck in a state that blocks learning.
What’s Really Driving Your Child’s Behavioral Challenges
Most parents can trace a timeline. Stressful pregnancy. Birth that didn’t go as planned. Early months were marked by colic, ear infections, and sensory issues that never resolved.
None of those are unusual. Taken alone, many kids handle them. But altogether? That’s The “Perfect Storm.”
The “Perfect Storm” isn’t one thing. It’s the combination of stress before birth, stress during birth, and stress after birth. When they add up early and often, they shift your child’s developing nervous system into that stuck, dysregulated, easily overwhelmed state – and it gets stuck there.
Prenatal Stress
During pregnancy, your baby’s nervous system is developing rapidly – and it’s sensitive to stress. The umbilical cord is an electrical connection between your nervous system and your baby’s. So when dealing with prenatal stress, cortisol and other stress hormones can cross the placental barrier.
Research on prenatal stress shows that prolonged exposure during sensitive developmental windows can alter how a child’s Autonomic Nervous System functions. They’re not starting from neutral – they’re starting where fight-or-flight is already the default.
Birth Trauma
Modern birth interventions, while often medically necessary, can create physical stress that overwhelms a baby’s capacity to adapt. C-sections, forceps, vacuum extraction, rapid or prolonged labor – these can create trauma to your baby’s upper neck and brainstem.
Additionally, the use of pitocin and induction procedures creates a surge of sympathetic stress for both mom and baby, often leading to nervous system dysregulation right out of the gates.
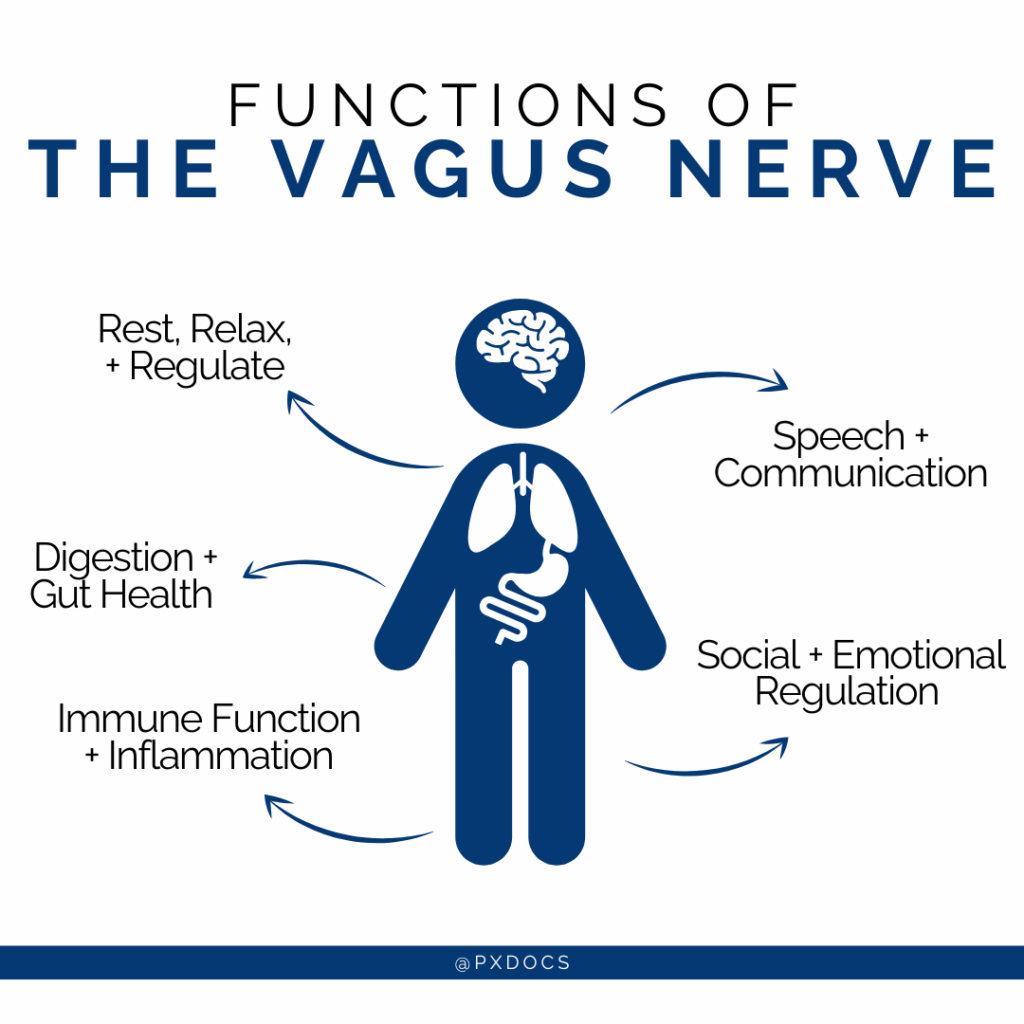
The vagus nerve, which controls digestion, immune function, social engagement, and the ability to calm down, is particularly vulnerable during birth. When physical trauma occurs, it creates what chiropractors call subluxation.
Subluxation keeps the nervous system stuck in survival mode. Sensory input is heightened, the amygdala remains on alert, and the prefrontal cortex – the part of the brain responsible for focus, emotional regulation, and behavior – struggles to stay engaged. Until that balance is restored, behavior strategies often fall short because the brain is busy protecting rather than learning.
This isn’t about blame. Many interventions are necessary. The point is to understand that your child’s nervous system may have experienced stress that sets them up for dysregulation, making it more difficult for them to respond to and benefit from traditional behavioral therapy and coping mechanisms.
Early Childhood Stressors + Toxic Overload
Our kids today face unprecedented stressors: environmental toxins, frequent antibiotics (which disrupt gut microbiome), chronic ear infections, other medications, 80+ vaccinations, food additives, falls, and repeated illnesses. Then add things like TV and technology, which many children are exposed to at a very young age – and we can start to see why their nervous systems are so easily overwhelmed, even if pregnancy and birth were uneventful.
The Result
Your child’s nervous system gets stuck in sympathetic dominance – gas pedal stuck on, brake pedal broken. The vagus nerve isn’t working properly. Brain centers associated with anxiety and overwhelm are overstimulated, and the ones in charge of focus and regulation are suppressed.
This explains why some kids bounce back while others struggle. It’s not about genetics or willpower – it’s about stress load and neurological function.
Some kids’ nervous systems have the capacity to handle modern stress. Others get overwhelmed during sensitive developmental windows and never fully recover.
The Physical Reality Behavioral Approaches Miss
There’s a fundamental misunderstanding: if your child can behave appropriately sometimes, they should do it all the time. That inconsistency is a choice, right?
Wrong. When your child’s nervous system shifts states, their access to skills changes.
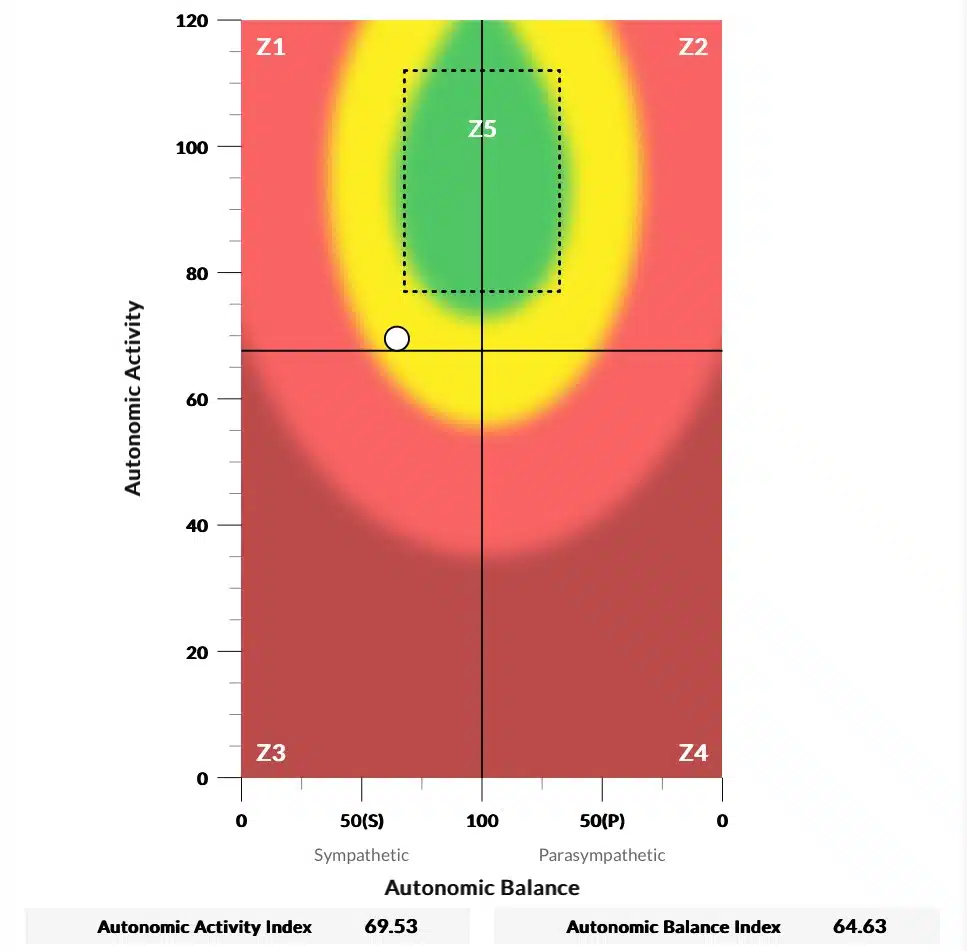
Heart rate variability (HRV) measures the variation in time between heartbeats. High HRV means your nervous system is flexible and adaptable. Low HRV means your system is rigid, stuck.
Kids with behavioral challenges consistently show low HRV. Low heart rate variability correlates with difficulty regulating emotions, increased anxiety, ADHD signs, and behavioral rigidity. You can’t talk a stuck system into unsticking.
When your child’s HRV is low, their nervous system has very little margin. Small stressors create big responses. Recovery takes longer. The window of regulation is narrow and unpredictable.
[INSERT RAGING BULL HRV LOW AND LEFT]
The Gut-Brain Connection
Approximately 90% of your child’s serotonin is produced in their gut. While not all of that serotonin is used for the classic understanding of mood and emotional regulation, it’s still essential to brain function that the gut is doing its job properly as well.
Serotonin affects sleep, appetite, digestion, sensory processing, behavior, and emotional regulation. When your child’s gut is disrupted, antibiotics, constipation, food sensitivities, and inflammation, their brain doesn’t get the neurochemical support it needs.
The gut-brain axis is a two-way highway. An inflamed gut sends distress signals to the brain. Those signals create anxiety, irritability, brain fog, and behavioral dysregulation. This isn’t psychological – this is inflammatory molecules creating real, physical changes in brain function.
The vagus nerve is the main communication pathway between the gut and the brain. When that nerve is dysfunctional (from birth trauma), the gut-brain communication breaks down. Brain problems create gut problems. Gut problems create brain problems. The cycle reinforces itself.
Measuring What Matters
Behavioral therapy relies on what can be observed. Did meltdowns decrease? Is sleep better? Those are important, but they’re subjective or symptom-based indicators – not accurate measurements of brain function and nervous system regulation.
That’s why we do things differently at PX Docs and not only measure subjective progress via parents’ reports as we go along, but also, most importantly, we track real functional change within the nervous system itself. We do so using an incredible piece of cutting-edge technology called the INSiGHT Scans, which directly measures nervous system function.
These scans have three (3) components and individual scans:
- Heart Rate Variability (HRV) measures sympathetic/parasympathetic balance. It shows whether your child’s system is stuck in fight-or-flight, whether they have flexibility to adapt to stress, and whether their body has any reserves left.
- Surface Electromyography (sEMG) assesses tension and altered neuro-sensori-motor dysfunction that may be present within the nervous system. Kids with behavioral challenges often show both sympathetic dominant tension patterns, and areas of asymmetry and exhaustion – which further leave the brain “wound up and worn out” from the altered sensory input and information.
- Thermal Scanning uses infrared sensors to measure temperature differences along the neurospinal system, indicating dysautonomia, an Autonomic Nervous System imbalance. This scan shows us areas of regional dysautonomia and alterations in gut, immune, and adrenal dysfunction as well – all of which can play a role in behavioral issues.
These three scans create a complete picture of nervous system function (or dysfunction). Often, when parents see their child’s INSiGHT Scans and have the findings explained to them, they become emotional because they can finally see what’s going on inside their child’s brain and body, and things make so much more sense.
Here’s another incredible benefit of these scans – they show changes before behavioral symptoms change, and they help us determine whether or not real lasting change is happening within the brain and nervous system itself.
When you start addressing nervous system dysfunction, the scans improve first. The system starts regulating, adapting, and gaining flexibility – and these changes show up on objective measurement before your child’s behavior visibly shifts.
The scans answer questions and provide symptom tracking, such as: Is my child’s nervous system actually changing? Is the intervention working even though I don’t see behavioral improvements yet? It’s the difference between driving blind and having GPS.
Take Casey and his emotional behavior challenges. His family tried everything to help him — talking through feelings, practicing coping strategies, and reassuring him that big emotions were okay — but nothing seemed to truly help. His meltdowns still came out of nowhere, leaving everyone confused and overwhelmed.
When they visited their local PX Docs office, they finally discovered why: Casey’s nervous system was stuck in a dysregulated state. Seeing his neurological scans brought clarity and relief.
With consistent chiropractic care, Casey transformed. He began expressing himself before a meltdown, his happiness returned, and he started thriving at home, in school, and in sports. Now, his family says finding PX Docs has truly changed their lives.
Finding Hope When Behavioral Therapy Hasn’t Been Enough
Behavioral therapy’s “failure” didn’t reveal that your child is broken. It revealed a deeper truth – your child’s challenges were never just behavioral to begin with.
When the nervous system is dysregulated, when the “Perfect Storm” has overwhelmed your child’s capacity to adapt, no amount of skills training can override the physiology keeping them stuck.
But here’s the hope – when you address the nervous system first, everything else changes and improves as well!
The neurologically-focused, root cause approach isn’t about creating workarounds or just coping with a dysregulated system – it’s about restoring nervous system function so your child’s body can finally regulate, process, adapt, and heal.
If you’ve tried everything and still feel stuck, you’re not alone – and you’re not out of options. We’ve walked this journey with thousands of families, helping them understand what’s really driving their child’s behavior challenges and creating the foundation that allows other therapies to finally work.
If you’re ready to address the foundation rather than just trying to better cope with the symptoms, visit the PX Docs Directory and find a Neurologically-Focused Chiropractor near you. These practitioners not only use the INSiGHT Technology and clinical protocols that help vastly improve quality of life for your child and entire family, but they also provide a supportive environment of understanding and empowerment.
Use the link above to book your consultation with a local PX Doc right away!