Mast cell activation syndrome (MCAS) is a complex condition that often leaves families managing antihistamines, epinephrine auto-injectors, and long lists of triggers while reactions continue to appear without clear patterns. Many clinicians describe MCAS as a chronic condition with symptom-focused management, and the underlying cause can feel frustratingly unclear.
What’s often overlooked is that mast cell activity doesn’t operate in isolation. The immune system is closely connected to the nervous system, particularly the vagus nerve, the main “brake pedal” that calms inflammatory responses. Understanding this connection can help explain why mast cells become hypersensitive in some individuals.
This article covers the signs, diagnosis, and care. But we’ll also explain the nervous system dysfunction that creates the environment for mast cells to become hypersensitive.
What is Mast Cell Activation Syndrome (MCAS)?
Mast cell activation syndrome is a rare condition in which mast cells, a type of white blood cell, release their chemical mediators too readily and without a clear trigger. In healthy people, mast cells release histamine and other chemicals only when there’s a real threat. In MCAS, these cells react to things that shouldn’t cause problems: temperature changes, stress, exercise, leftover foods, aged meat, or no identifiable trigger at all.
You might see flushing, low blood pressure, diarrhea, and shortness of breath all happening together. These reactions can range from uncomfortable to life-threatening, with anaphylaxis being a real risk.
MCAS is often confused with mastocytosis, but they’re different. Mastocytosis involves an abnormal accumulation of mast cells in body tissues. MCAS is about activation; the mast cells you have are releasing their contents when they shouldn’t.
MCAS often shows up alongside POTS and Ehlers-Danlos Syndrome. That clustering isn’t random; there’s a nervous system connection we’ll explain later.
Mast Cell Activation Syndrome Signs
MCAS signs can affect virtually any part of the body. The reactions are unpredictable; what triggers a severe episode one day might not cause problems the next.
- Skin: Flushing, hives, and swelling can appear suddenly. The flushing might start on the face and spread down the neck and chest. Another common symptom is varicose veins.
- Gastrointestinal: Diarrhea and vomiting can happen suddenly, sometimes severe enough to cause dehydration. Many people deal with chronic nausea, cramping abdominal pain, and bloating. Food sensitivities multiply.
- Cardiovascular: Low blood pressure is common during episodes and can cause dizziness or lightheadedness. Heart rate might spike without explanation. Some people faint, especially when standing up.
- Respiratory: Shortness of breath, wheezing, and chest tightness are classic signs. The airways can narrow during an episode.
- Neurological: Brain fog, difficulty concentrating, memory problems, headaches, and mood changes can all occur during reactions.
The defining feature is that symptoms involve multiple parts of the body during the same episode. Many people notice MCAS signs look similar to dysautonomia or POTS; there’s a reason these conditions appear together.
Conditions Often Seen Paired With Mast Cell Activation Syndrome:
- Ehlers-Danlos Syndrome (EDS)
- POTS (Postural Orthostatic Tachycardia Syndrome)
- Fibromyalgia
- Chronic Fatigue Syndrome (ME/CFS)
- Thyroid Problems
- Endometriosis and PCOS
- Dysautonomia
How Mast Cells Work in Your Body
Mast cells are a type of white blood cell that acts as your immune system’s first responders. They’re stationed throughout your body, in the skin, digestive tract, lungs, around blood vessels, and in connective tissues.
When mast cells detect danger—bacteria, viruses, parasites, or allergens—they release stored chemical mediators. Histamine is the most well-known, but mast cells also release tryptase, prostaglandins, and leukotrienes. These create the signs we recognize as an allergic reaction.
In a healthy immune system, this response is proportional and controlled. In MCAS, the activation threshold is unfortunately set too low. Mast cells release histamine and other chemicals in response to things that shouldn’t trigger them, but do.
What conventional medicine doesn’t explain is that mast cell activation isn’t random. These cells respond to signals from the Autonomic Nervous System. When that communication system is dysregulated, mast cells become hypersensitive.
Mast Cell Activation Syndrome Causes and Triggers
- Primary MCAS involves genetic mutations in the mast cells themselves, particularly the KIT gene mutation (D816V). This is less common.
- Secondary MCAS happens when something else causes mast cells to become overactive—infections, autoimmune conditions, or other underlying diseases.
- Idiopathic MCAS is the most common and most frustrating form. “Idiopathic” means doctors can’t identify a specific cause. You or your child’s mast cells are clearly overactive, but standard testing doesn’t reveal why.
Common triggers include temperature changes, physical exertion, stress, certain foods, medications, fragrances, chemical exposures, insect stings, and infections. Triggers can vary wildly and change unpredictably.
Here’s where conventional medicine stops: at “idiopathic” or “unknown cause.” But findings increasingly point to nervous system dysfunction as a missing link. When the Autonomic Nervous System is dysregulated, stuck in chronic “fight or flight,” it creates an environment where mast cells become hypersensitive to normal stimuli.
How is Mast Cell Activation Syndrome Diagnosed?
Diagnosing MCAS requires meeting three criteria:
- Symptoms affecting two or more organ systems simultaneously
- Elevated mast cell mediators (tryptase, histamine) during episodes
- Improvement with medications that block mast cell mediators
Tryptase is the most commonly measured marker, but timing matters. Levels spike during a reaction but return to normal within hours. The blood draw needs to happen during or shortly after an episode.
The diagnostic journey often takes years. Many people see multiple specialists before finding a board-certified allergist or immunologist familiar with MCAS.
What conventional testing misses is the underlying nervous system dysfunction driving mast cell hypersensitivity. This is where finding and researching the root cause is essential, and where asking questions like “Why would my body be reacting this way?” is essential.
Mast Cell Activation Syndrome Medical Care Options
- Antihistamines form the foundation. Western Medicine Doctors typically prescribe both H1 antihistamines (loratadine, cetirizine, fexofenadine) and H2 antihistamines (famotidine, ranitidine) to target different histamine receptors.
- Mast cell stabilizers like cromolyn sodium (Gastrocrom) try to prevent mast cells from releasing their mediators in the first place.
- Leukotriene inhibitors like montelukast (Singulair) help with respiratory signs and inflammation (used off-label for MCAS).
- Omalizumab (Xolair) is given as an injection for severe cases that don’t respond to other care plans (off-label use).
- Epinephrine auto-injectors. It is recommended that every person with MCAS have one accessible at all times.
These medications help manage symptoms day to day. But they don’t address why your mast cells became hypersensitive. They’re managing the signs, not changing the environment that created the problem.
The Vagus Nerve and Mast Cell Connection
Here’s what conventional medicine is missing: the immune system is controlled by the nervous system, specifically the vagus nerve.
The vagus nerve runs from the brainstem through the neck into the chest and abdomen. It’s the main component of the Parasympathetic Nervous System. This is the “brake pedal” that calms your body down. One of its critical jobs is controlling inflammatory responses.
Think of the nervous system like a car. The Sympathetic Nervous System is the gas pedal (activates during danger). The Parasympathetic Nervous System is the brake pedal (calms everything down).
In people with MCAS, the gas pedal is stuck down. Their nervous system interprets normal things as threats. The mast cells respond by releasing histamine and other chemicals. But the brake pedal (vagus nerve) can’t calm the response down.
This constant “threat mode” is sympathetic dominance. MCAS, POTS, Dysautonomia, and Ehlers-Danlos Syndrome often appear together because all three share the same root: Autonomic Nervous System dysfunction.
How Mast Cell Activation Syndrome Develops: The “Perfect Storm”
MCAS doesn’t develop overnight. It’s almost always the result of the “Perfect Storm” stressors that accumulate over time and dysregulate the nervous system.
Stage 1: Prenatal and Birth Stress
Let’s take it way back to your mom’s pregnancy and birth with you. Prenatal stress can affect fetal nervous system development. Birth trauma, difficult labor, forceps, vacuum extraction, or cesarean section can cause physical trauma to the baby’s upper cervical spine and brainstem region, where the vagus nerve exits. This creates subluxation: neurospinal misalignment, restricted movement (fixation), and neurological interference.
Stage 2: Early Childhood And Teenage Stressors
Repeated ear infections, antibiotic use, poor sleep, digestive issues, birth control, medications, hormonal imbalances, vaccines, medical interventions, and emotional stress add to the nervous system’s burden. When stressors come too frequently, the nervous system never returns to baseline.
Stage 3: Nervous System Dysregulation
The nervous system runs in “fight or flight” mode for so long that the immune system becomes hypersensitive. Mast cells lose their ability to distinguish between real threats and harmless stimuli. This is when signs emerge. This can lead to other diagnoses that come along with MCAS.
Conventional medicine sees the mast cell problem but misses the nervous system dysfunction that created the environment for those mast cells to go haywire.
Diving More Into Traumas, Toxins, and Thoughts
For over a century, chiropractors have educated patients about what we call the “3Ts” – trauma, toxins, and thoughts. This framework helps us understand how various environmental and life stressors accumulate to impact immune health and trigger MCAS symptoms. For people with MCAS, these stressors directly affect the nervous system’s ability to regulate mast cell function and immune responses.
Neurologically-Focused Chiropractors examine how these physical, chemical, and emotional stressors lead to an overstressed, imbalanced, and dysregulated nervous system. While everyone encounters physical injuries, toxic exposures, and emotional stress throughout life, MCAS often develops when these 3Ts appear early, frequently, and intensively during critical developmental periods.
A single physical trauma, exposure to environmental toxins, or stressful event alone is not as likely to trigger MCAS. However, when a person experiences multiple stressors during crucial developmental periods, their nervous system’s ability to adapt and overcome these challenges becomes suppressed and dysfunctional. This is particularly true for people who experience birth trauma/intervention, frequent early antibiotic use or toxin exposure, and high stress environments – all key components of the “Perfect Storm” that often precedes MCAS development.
This decreased resilience and limited adaptability create the perfect conditions for MCAS to develop. When the nervous system becomes overwhelmed and dysregulated, it shifts into sympathetic “fight or flight” overdrive. This state triggers increased inflammation, hypersensitive immune responses, and overuse of mast cells – all hallmark features.
Understanding the role of chronic stress, the 3Ts, and nervous system dysregulation is crucial because both sides of the healing equation must be addressed:
- First, we must heal and repair any damage to the nervous system. Subluxation and nervous system dysregulation often create a vicious cycle of sympathetic dominance, leading to increased inflammation and reactivity. Neurologically-focused chiropractic adjustments first release this stuck stress pattern, then work to restore optimal neurological function and balance.
- Second, while we can’t erase past traumas or stressors that contributed to MCAS development, we can support more effective healing by addressing current physical, chemical, and emotional well-being. This includes reducing exposure to common triggers and environmental toxins that can further stimulate an already overactive immune and nervous system response.
Fortunately, more people are recognizing how environmental toxins impact their immune and nervous system health.
If you suspect the 3Ts have contributed to your MCAS, focus on these key action steps:
- Reduce exposure to environmental triggers and pro-histamine foods and toxins, particularly fragrances, hung and aged meats, fast food, leftovers, fermented foods, high-inflammatory foods, alcohol, and caffeine.
- Support nervous system function and regulation through Neurologically-Focused Chiropractic Care to help restore proper communication between the brain and mast cells/immune system.
Remember that just as MCAS develops over time through accumulated stress and nervous system dysfunction, healing through natural and neurological approaches also requires patience and consistency. By addressing both the nervous system dysfunction and environmental factors, many people find they can reduce their reliance on medications and better manage their health naturally.
Addressing MCAS at the Neurological Level
Neurologically-Focused Chiropractors examine the nervous system itself. INSiGHT scans measure five markers and more:
- How well the two sides of the nervous system communicate
- Sympathetic versus parasympathetic balance
- Autonomic Nervous System function
- Neuromuscular tension, energy, and hormonal imbalances
- How adaptable and resilient the body is to outside stressors and triggers
These scans reveal the nervous system dysfunction that contributes to immune dysregulation. People with MCAS typically show high sympathetic activity (gas pedal floored), low vagal tone (weak brake pedal), neurological confusion and exhaustion, and tension patterns throughout the neuromuscular system.
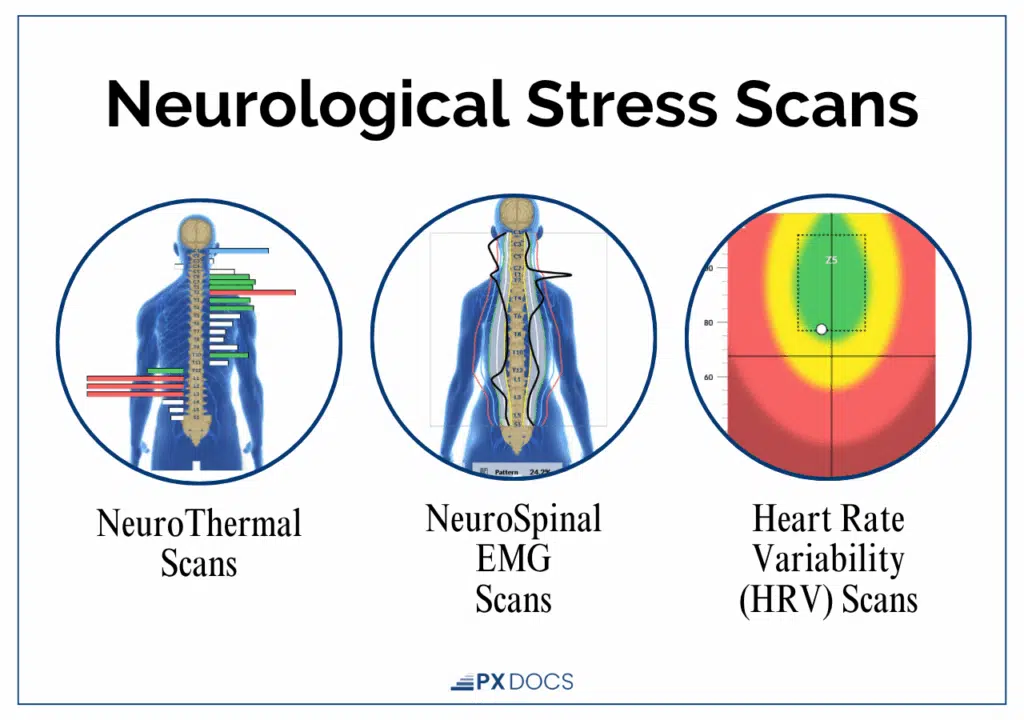
The INSiGHT technology has not been evaluated by the FDA and is not intended to diagnose, treat, cure, or prevent any disease.
Neurologically-Focused Chiropractic Care doesn’t treat or cure MCAS; it addresses nervous system dysfunction that contributes to immune dysregulation. Specific adjustments remove subluxation interference, particularly where the vagus nerve is most vulnerable.
As subluxation is reduced and neurological adaptation is restored, vagal tone typically improves. The brake pedal starts working better. This shifts the nervous system out of chronic sympathetic dominance.
The scans can improve before the symptoms do. People often see nervous system regulation on INSiGHT scans weeks before they notice fewer reactions. This is healing from the inside out. We re-scan frequently to track progress.
Neurologically-Focused Care addresses the root cause. The nervous system dysfunction created the environment for mast cell hypersensitivity, and needs to heal before other systems can come back online. There is a specific order of healing that the body goes through, and the nervous system is the foundation.
Finding Hope and Answers for Mast Cell Activation Syndrome
If you have MCAS, you know the daily challenge of managing triggers and keeping epinephrine close by. Medications can help in the short term. Trigger avoidance helps. But addressing nervous system dysfunction through Neurologically-Focused Chiropractic Care can help your body regulate from the inside out, building a stronger foundation rather than just managing symptoms.
The “idiopathic” label doesn’t have to be a dead end. The “Perfect Storm” of prenatal stress, birth trauma, and childhood + teenage stressors can create nervous system dysfunction. That dysfunction drives mast cell hypersensitivity. And the nervous system dysfunction should be addressed so the body has the opportunity to adapt and heal as it was designed to.
Finding a PX Docs provider through our directory gives you access to the missing piece that conventional medicine sometimes overlooks. The combination of medical management for traits and Neurologically-Focused Care for root causes provides a more complete path forward.
When the nervous system shifts from sympathetic dominance back toward balance, the immune system follows. Mast cells become less reactive. Triggers don’t provoke the same intense responses.