Here’s what your OB won’t tell you: the modern American pregnancy experience, with its constant monitoring, interventions, tests, and fear-based messaging, creates chronic prenatal stress that affects your nervous system. And that stressed nervous system? It’s directly programming your baby’s developing nervous system.
Before we dive in, we never want you to ever feel guilty about anything, especially when you didn’t know. We’ve been there too. It’s now about going forward, learning more, sharing our stories, and understanding what happened so we can all better understand what our children might need now.
The Modern Pregnancy Reality Nobody Talks About
Your great-grandmother had maybe four or five prenatal appointments total during her pregnancy. She didn’t have routine ultrasounds, genetic testing, or glucose challenges. When she went into labor, she either delivered at home or showed up at the hospital when contractions were close together.
Today? We, women, are having 12-15 routine appointments, multiple ultrasounds, various blood draws, glucose tolerance tests, Group B Strep testing, non-stress tests if you’re “high-risk,” and constant monitoring that sends a clear message: something could be wrong at any moment.
The medical system calls this “better care.” And yes, some interventions save lives. Some new technologies and protocols are amazing and necessary for some who may need them. But what gets missed completely is the neurological cost of treating every pregnancy like a medical emergency waiting to happen.
Your body experiences each appointment, each test, each “let’s keep an eye on that” comment as a stress signal. And stress doesn’t just affect your mood. It affects your Hypothalamic-Pituitary-Adrenal (HPA) axis, your autonomic nervous system, and your baby’s developing nervous system.
The Trimester-by-Trimester Timeline: What You Actually Experience
First Trimester (Weeks 1-13): The Foundation Is Set
What’s Happening in Your Body: Pregnant women are usually exhausted in a way they’ve never experienced before. You might have morning sickness, food aversions, or constant nausea. Your body is building a placenta, a brand-new organ, from scratch. Hormones are surging. Your digestive system slows down (hello, constipation).
Your nervous system is working overtime trying to support this massive developmental process while you’re still expected to function normally at work, at home, in life.
What’s Happening at Traditional OB Appointments:
Week 6-8: First Visit
- Confirmation ultrasound (checking for heartbeat, dating)
- Full medical history review
- Multiple tubes of blood drawn (blood type, Rh factor, complete blood count, rubella immunity, hepatitis B, syphilis, HIV, sometimes thyroid function)
- Genetic carrier screening offered (cystic fibrosis, spinal muscular atrophy, others)
- Pap smear if you’re due
- “Here’s your list of things to avoid” conversation (which feels endless)
You leave either relieved or worried, depending on what they found or didn’t find.
Week 10-13: The Genetic Testing Discussion
- Non-invasive prenatal testing (NIPT) offered – cell-free DNA screening
- First trimester screening (blood work + nuchal translucency ultrasound)
- If you’re over 35, you’re hearing the term “advanced maternal age” or “geriatric pregnancy” (because that’s not stressful at all)
- Discussion of amniocentesis or CVS if any concerns arise
The Stress Reality: Every test comes with waiting. Waiting for results. Checking the patient portal obsessively. Googling what every number means. Your nervous system interprets this waiting as a threat assessment. Your HPA axis stays activated, releasing cortisol, keeping you in sympathetic (“gas pedal”) mode instead of the parasympathetic (“brake pedal”) rest-and-digest state your body needs for optimal development. Not to mention, do any of these tests have effects on your growing baby?
Second Trimester (Weeks 14-27): The “Easy” Phase That Isn’t Always Easy
What’s Happening in Your Body: You might have more energy, which everyone tells you means this is the “best trimester.” Your body is growing rapidly now. Your center of gravity shifts. Round ligament pain shows up. You’re feeling movement, which is amazing, but also makes everything feel more real and sometimes more anxiety-producing.
What’s Happening at Traditional OB Appointments:
Week 16-18: Regular Check-in
- Fundal height measurement
- Fetal heart tone check with Doppler or Ultrasound
- Blood pressure monitoring
- Weight check (with judgment if you’ve gained “too much” or not enough)
- Sometimes, additional blood work for a quad screen
- Discussion of anatomy scan coming up
Week 20: The Anatomy Scan. This is the big one. The detailed ultrasound where they’re looking at every structure, every organ, measuring everything. You’re excited to see baby, but also holding your breath, hoping they don’t find anything concerning.
- 30-45 minutes of ultrasound imaging
- Detailed measurements of brain, heart, kidneys, limbs, and spine
- Placenta location check
- Amniotic fluid assessment
- Gender reveal if you want it
- The waiting while the tech is silent, knowing they can’t tell you if something’s wrong
- Then waiting for the doctor to review and call with results
Week 24-28: Glucose Testing Time. Here’s where it gets particularly stressful for many moms:
- You drink the glucose solution (Glucola) – 50g or 75g of sugar and other toxic ingredients
- They’re testing for gestational diabetes
- If you fail the one-hour test, you come back for the three-hour glucose tolerance test
- More fasting, more blood draws, more waiting for results
- If diagnosed with gestational diabetes, entire new protocol begins: finger pricks multiple times daily, dietary restrictions, possibly medication, labeled “high-risk”, induction talk
Week 28: The Rh Factor Decision
- If you’re Rh-negative, you get the RhoGAM shot
- Another injection, another intervention
- More waiting to see if there are any reactions
Monthly Appointments Continue: Every 4 weeks through week 28, you’re going in for:
- Blood pressure checks
- Urine screening (protein and glucose)
- Weight monitoring
- Fundal height measurement
- Fetal heart rate monitoring
- “Any concerns?” conversations that sometimes help but often just add to your mental load
The Stress Reality: By now, if you’ve been flagged for anything – slightly elevated blood pressure, measuring ahead or behind, any concerning findings on ultrasound, failed glucose test – you’ve been moved to “high-risk” status. This means more appointments, more monitoring, more interventions. Your nervous system is getting the message loud and clear: something is wrong, stay on high alert. Not to mention the other stressors, like toxins that may come with the interventions as well.
Third Trimester (Weeks 28-40+): The Final Stretch That Feels Endless
What’s Happening in Your Body: You’re exhausted again, but in a different way. Sleep is difficult. Your body aches. You’re having Braxton Hicks contractions. Heartburn is constant. You’re peeing every hour. You’re worried about labor. You’re worried about being a mom. You’re worried about everything.
Your nervous system is already taxed from seven months of pregnancy, and now you’re adding the stress of “what if I go into labor right now,” combined with “what if I never go into labor.”
What’s Happening at Traditional OB Appointments:
Weeks 28-36: Appointments Every 2 Weeks
- All the same checks as before (blood pressure, weight, fundal height, heart rate)
- More frequent monitoring means more opportunities to hear “let’s keep an eye on that”
- Additional blood work (complete blood count, checking for anemia)
- More discussions about birth plan (which often get dismissed if not aligned with provider preferences)
Week 35-37: Group B Strep Test
- Vaginal and rectal swab
- If positive (which 25% of women are), you’re told you need IV antibiotics during labor
- More medication, more intervention, more things to worry about during birth
- If you wanted a natural birth, this complicates things
Vaccines Offered And Encouraged Throughout Pregnancy By Traditional OBs:
- Whooping Cough Vaccine
- COVID-19 Vaccine
- The FLU Shot
- RSV Vaccine
- HEP A and B
Week 36+: Weekly Appointments and Final Monitoring. Now you’re going every single week for routine monitoring, cervical checks (often uncomfortable), discussions about induction deadlines, and pressure about not going past 40-41 weeks. Every appointment comes with “still pregnant?” energy from the staff.
If showing any complications: non-stress tests twice weekly (20-40 minutes hooked to monitors), biophysical profiles, amniotic fluid checks, additional cervical exams, and daily kick counts at home. More monitoring equals more opportunities for anxiety.
The Induction Conversation: As you approach or pass your due date, the pressure intensifies: “Baby’s getting too big,” “Placenta is aging,” “Fluid is getting low,” “It’s safer to induce.” Fear-based messaging about stillbirth risk. Scheduling pressure. The message is clear: your body can’t be trusted to do this on its own.
The Stress Reality: You’re now seeing your provider weekly or more. You’re being monitored constantly. Your body is uncomfortable. You’re not sleeping well. Everyone is asking, “Still pregnant?” or telling you their birth horror stories. You’re worried about labor pain. You’re worried about complications. You’re worried about whether you’ll need interventions you wanted to avoid.
Your nervous system has been in fight-or-flight mode for weeks or months. This is the critical final developmental period for your baby’s brain, and your stress signals are constantly crossing the placenta.
Special Circumstances: When the Intervention Load Multiplies
If your pregnancy falls into any “special” category, the baseline stress described above gets amplified significantly:
High-Risk Pregnancies: Appointments every 1-2 weeks starting in the second trimester, maternal-fetal medicine specialists, non-stress tests as early as 28 weeks, possible medications (blood pressure, blood thinners, progesterone, insulin), biophysical profiles multiple times weekly, constant messaging about increased risk. Every appointment becomes a chance to hear bad news.
Multiples (Twins, Triplets): Everything above intensified – more frequent growth ultrasounds for each baby, earlier monitoring, additional risk labels (twin-to-twin transfusion, growth discordance), increased chance of bed rest, and earlier delivery discussions. You’re managing worry about multiple babies simultaneously.
IVF/IUI Pregnancies: Stress started before conception – months or years of failed cycles, hormone injections, frequent monitoring, financial strain, emotional trauma from losses, and financial stress. During pregnancy: continued progesterone supplementation for 10-12 weeks, extra early monitoring (sometimes weekly until 12 weeks), automatic high-risk labeling, and inability to relax after your body “failed” to conceive naturally. Your HPA axis dysregulation predates pregnancy.
“Geriatric” Pregnancies (35+): The label itself creates stress. Constant focus on age-related risk statistics, pressure for genetic testing, more frequent monitoring, assumption you’ll need interventions, lower threshold for induction, social messaging that you’ve “waited too long.” Most women over 35 have healthy pregnancies, but the medical system treats age as an automatic risk, creating stress where actual medical concern may not exist.
The common thread: your nervous system has been in fight-or-flight mode longer, with more intensity, and less opportunity for parasympathetic recovery. The prenatal programming of your baby’s nervous system reflects this cumulative load.
The Biology of Maternal Stress: What’s Really Happening
When you experience stress during pregnancy, it’s not just emotional. It’s biological, and it directly affects your baby.
Your HPA (Hypothalamic-Pituitary-Adrenal) axis responds to stress by releasing cortisol. Short bursts? Normal. Chronic elevation from weekly appointments, constant test results, and repeated “we need to keep an eye on this” messaging? Problem.
Your placenta has a protective enzyme (11β-HSD2) that converts active cortisol into inactive cortisone before reaching your baby. But chronic stress overwhelms this protection – active cortisol crosses the placenta and reaches your baby’s developing brain.
Your Autonomic Nervous System: The Gas and Brake Pedals
Think of your nervous system like a car with two pedals:
Gas Pedal (Sympathetic Nervous System):
- Fight-or-flight response
- Heart rate up, blood pressure up
- Digestion slows, and immune function is suppressed
- Energy mobilized for dealing with threats
- Designed for short-term crises
Brake Pedal (Parasympathetic Nervous System):
- Rest, digest, heal, grow
- Heart rate normal, digestion working
- Immune function optimal
- Energy directed to growth and repair
- Should be your default state during pregnancy
In a healthy system, you shift between them based on actual needs. But when you’re chronically stressed, your gas pedal is pressed down constantly. Your body thinks it’s being chased by a bear 24/7.
This is a problem because pregnancy and fetal development require parasympathetic dominance. Your baby needs you in rest-and-digest mode to develop optimally.
The Umbilical Cord: More Than a Nutrient Delivery System
Here’s what changes everything about understanding pregnancy stress.
That umbilical cord connecting you to your baby? Medical science focuses on its role in delivering oxygen and nutrients. That’s accurate. But there’s another level of communication happening that most doctors never mention.
Think of that umbilical cord as an electrical power cord, carrying the signals from your nervous system directly to your baby’s developing nervous system through the hormones in the blood.
When your nervous system is in fight-or-flight mode, those signals are transmitted to your baby’s developing nervous system. Your baby’s baseline “normal” is being established based on your nervous system state.
If your nervous system is chronically activated in sympathetic mode from months of stressful appointments, test results, and fear-based messaging, your baby’s nervous system is developing in that same state. They’re being pre-programmed for sympathetic dominance before they’re even born.
This isn’t genetics. This is nervous system programming during the most critical developmental window.
What’s Being Programmed in Your Baby’s Brain
During pregnancy, your baby’s brain is developing at an incredible rate. Critical structures are being formed:
Key Brain Structures Affected:
The amygdala (fear center) develops larger and more reactive; babies startle easily and struggle to calm down. The hippocampus (memory and learning) shows reduced volume, affecting learning ability and emotional regulation. The prefrontal cortex (executive control) develops altered connectivity, making it harder to control emotional responses. The vagus nerve forms with low tone under chronic stress, leading to poor regulation of the heart, lungs, digestion, immune system, and emotions. Neurotransmitter systems (serotonin and dopamine) are altered, affecting mood and emotional regulation throughout life.
The Research That Confirms This
A 2017 study published in Development and Psychopathology tracked mothers and children from pregnancy through age six. The findings were clear: babies born to mothers with high prenatal stress showed nervous systems that were 22% more reactive at six months old compared to babies of less-stressed mothers.
Twenty-two percent. That’s measurable, quantifiable nervous system dysregulation that started before birth.
These babies also showed:
- 8% lower levels of positive emotional engagement
- 8% lower self-regulation capacity
- Poorer recovery from stressors
- Greater risk for anxiety, depression, and behavioral problems as they grew
Other research has documented cognitive impacts, with children born after high-stress pregnancies scoring lower on IQ tests and showing increased rates of ADHD, anxiety, and autism spectrum characteristics.
The Perfect Storm: Stage 1 Begins Before Birth
At PX Docs, we call this “The Perfect Storm” – the accumulation of multiple stressors during critical developmental windows that overwhelm a child’s developing nervous system.
Most people think The Perfect Storm starts at birth with birth trauma. But we’ve learned it actually starts earlier.
Stage 1: Prenatal Stress and Programming
This is what you’ve been reading about. The foundation is set during pregnancy:
What Creates Prenatal Stress:
- Fertility struggles and treatments
- Chronic maternal anxiety or depression
- Major life stressors (job loss, relationship problems, death of a loved one, financial crisis)
- Medical complications during pregnancy
- High-risk status and increased monitoring
- Constant interventions and testing
- Fear-based obstetric messaging
- Lack of a support system
- Previous pregnancy loss or trauma
What Happens in Baby’s Nervous System:
- High cortisol passed through to baby
- Sympathetic dominance becomes baseline “normal”
- The vagus nerve develops with low tone
- Brain structures form in stress-adapted patterns
- Neurotransmitter systems establish stress-reactive patterns
Your baby enters the world with a nervous system that’s already compromised, already stuck in fight-or-flight mode, already programmed for dysregulation.
Why This Matters for What Happens Next
When birth trauma occurs (Stage 2 of The Perfect Storm), it hits a nervous system that’s already vulnerable. The physical trauma to the upper cervical spine, brainstem, and vagus nerve creates subluxation (physical misalignment combined with neurological interference).
But because the nervous system is already dysregulated from prenatal stress, the impact is worse. A baby with a resilient, well-regulated nervous system might handle birth trauma better. A baby who spent nine months developing in chronic stress mode with years of stress during preconception for mom and dad? They don’t have that resilience buffer.
Then early childhood stressors hit (Stage 3): antibiotics, environmental toxins, infections, vaccines, and standard childhood stress. Again, a compromised nervous system can’t handle these normal stressors as well as a regulated one.
It’s not one thing. It’s the accumulation during the most critical developmental windows. This explains why siblings can have such different outcomes. They each had a different Perfect Storm severity.
Recognizing the Signs: What This Looks Like
During Pregnancy
You might be reading this while pregnant, wondering if your baby’s nervous system is being affected. These patterns suggest increased risk:
Maternal Stress Indicators: Diagnosed anxiety or depression, mental health medications, history of trauma or PTSD, major life stressors, high-risk status, frequent monitoring and interventions, constant worry about baby’s health, difficulty relaxing, poor sleep throughout pregnancy, feeling disconnected from pregnancy or baby, no support system, fertility treatments, or previous pregnancy loss.
Physical Signs: Persistent elevated blood pressure, difficulty managing blood sugar, chronic tension or pain, digestive issues, frequent illness, or inability to manage weight appropriately.
At Birth and in Early Infancy
If your baby was affected by prenatal stress, you’ll often see signs immediately:
Right Away:
- Difficulty latching (often worse on one side)
- Nursing is painful for you despite a “correct” latch
- Baby seems tense even during sleep
- Excessive crying that nothing soothes
- Arching back during feeding or holding
- Torticollis (head consistently tilted to one side)
- Plagiocephaly (flat spots developing on the head)
- Startles very easily
- Trouble sleeping or staying asleep
- Physical tension you can feel when holding them
First Few Months:
- Colic (inconsolable crying for hours)
- Reflux that doesn’t respond to medication
- Chronic constipation or digestive issues
- Nursing difficulties continuing
- Sleep that never improves
- Sensory sensitivities already apparent
- Difficulty calming down once upset
- Poor weight gain despite adequate feeding
- Frequent illness or infections
- Motor development delays
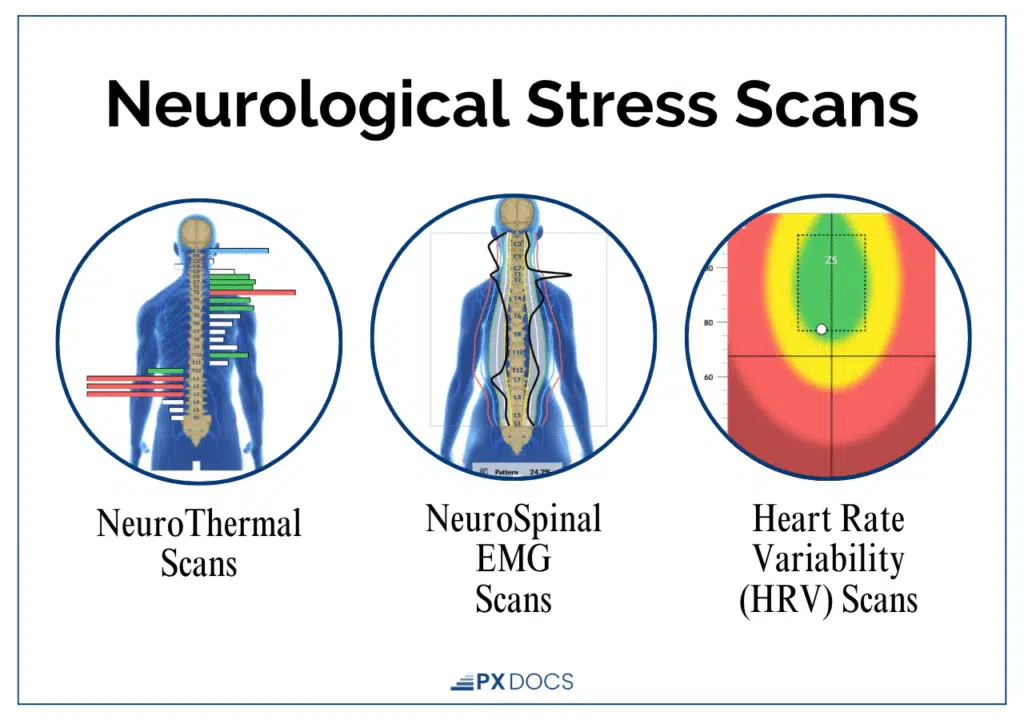
Your pediatrician will likely say “it’s normal” or “they’ll grow out of it.” But when we scan these babies with INSiGHT scan technology as PX Docs, we consistently see the same pattern: sympathetic nervous system dominance, parasympathetic suppression, and low vagal tone.
The Progression Pattern
These signs don’t improve with time; they evolve. The same nervous system dysregulation that causes colic at 2 months becomes constipation at 6 months, sensory sensitivities at 18 months, ADHD signs at 5 years, and anxiety by 10 years. The neurology doesn’t change – the medical system just gives it different names as your child grows.
What You Can Do: During Pregnancy and After
If You’re Currently Pregnant
First, reading this doesn’t mean it’s too late! Awareness is the first step to change, and there’s still time to help your nervous system shift toward better regulation.
Focus on Parasympathetic Activation and Consider Neurologically-Focused Prenatal Chiropractic Care:
This is where we differ from typical prenatal chiropractic. We’re not just adjusting your pelvis for an easier birth or to improve baby positioning (though that helps and is great). We’re addressing subluxation that affects your vagus nerve and autonomic nervous system.
When we adjust a pregnant mom, we’re helping shift her nervous system toward parasympathetic dominance. We’re supporting vagal tone. We’re reducing the stress signals being transmitted to baby.
We can do Neurological INSiGHT scans that show exactly how your nervous system is functioning:
- Where sympathetic dominance is highest
- How well your parasympathetic system is working
- Where subluxation exists
- How your body is adapting to stress
Then we create a care plan focused on nervous system regulation, not just symptom relief.
Advocate for Yourself in Medical Appointments:
- You can decline tests that aren’t medically necessary
- You can ask, “What changes if this result is abnormal?” before agreeing to testing
- You can space appointments if you’re low-risk
- You can switch providers if yours is increasing your stress
- You can say no to induction if there’s no medical emergency
- You can trust your body more than fear-based messaging
If Your Baby Has Already Been Born
It’s not too late. Neuroplasticity is real. Your child’s nervous system can change, and we see it happen all of the time! Check out our success stories!
Get Assessment First:
Don’t guess about what your child needs. Find a PX Doc trained in Neurologically-Focused Chiropractic Care who can do INSiGHT scanning.
Address the Foundation:
Neurologically-Focused Chiropractic Care for your baby or child addresses:
- Subluxation from preconception, prenatal stress, and birth trauma
- Sympathetic nervous system dominance
- Parasympathetic suppression or exhaustion
- Vagal tone dysfunction
- Neurological interference blocking brain-body communication
The adjustments are incredibly gentle and specific to what your child’s nervous system needs.
Why This Works When Other Things Haven’t:
Here’s the key: if your child’s nervous system is stuck in fight-or-flight mode from prenatal programming, their body physically cannot:
- Digest properly (parasympathetic function)
- Sleep deeply (parasympathetic function)
- Regulate emotions (vagal function)
- Fight infections effectively (immune function tied to autonomic balance)
- Learn and focus optimally (requires nervous system flexibility)
- Calm down after upset (requires intact brake pedal)
You can do:
- Dietary changes (which help but require digestion to work)
- Supplements (which require absorption and metabolism)
- Behavioral therapy (which requires emotional regulation capacity)
- Sleep training (which requires nervous system ability to shift to parasympathetic state)
- Occupational therapy (which requires sensory processing function)
All of these can help. But if the foundational nervous system dysfunction isn’t addressed, then we’re trying to build on a cracked foundation.
Once we help the body remove the subluxation and restore neurological function, the body’s healing capacity emerges. Then all those other interventions work better because the foundation is solid.
The Order Matters:
Wrong order: diet changes → supplements → therapy → medication → finally chiropractic (“I wish we’d done this first”). Right order: address nervous system dysfunction with Neurologically-Focused Chiropractic Care first, then add diet changes, supplements, and therapies once regulation improves. We’re not against other interventions – we just know that the order matters most!
Your Next Step:
Visit our PX Docs directory to find a trained practitioner near you. Get INSiGHT scans. See the actual neurological dysfunction. Get a clear care plan focused on nervous system regulation.
Whether you’re still pregnant and want to optimize your baby’s development or your child is already here, the path forward is the same: address the nervous system dysfunction at its source.
The Perfect Storm started before birth. The solution starts with understanding what really happened and what your or your child’s nervous system actually needs.