You’re exhausted. You’re worried. And now someone’s telling you to “just relax” for your baby’s sake—as if you haven’t tried that already.
Between the nausea, the fear, the financial pressure, and everyone’s advice, you’re barely holding it together. The guilt about stress during pregnancy might be worse than the stress itself. If you’re searching for answers about how stress affects your baby, you’re in the right place. Up to 70% of pregnant women report experiencing significant stress.
Most articles mention cortisol and preterm birth, then suggest prenatal yoga. What they don’t explain is the neurological mechanism—how your stress creates lasting changes in your baby’s developing nervous system.
That umbilical cord isn’t just delivering nutrients and oxygen. It’s an electrical connection between your nervous system and your baby’s developing nervous system. When you’re stuck in stress mode, your baby’s nervous system is learning that stressed state as “normal” during the most critical window of brain development.
This article explains fetal programming and how stress during pregnancy can affect your child’s health trajectory for years to come. More importantly, it offers root-cause solutions beyond managing symptoms.
What Is Stress During Pregnancy?
Stress is your body’s natural response to challenges. When stressed, your body releases hormones like adrenaline and cortisol to help you cope. This is normal and adaptive.
But there’s a big difference between normal pregnancy stress and chronic stress that affects your baby’s development.
Normal Stress vs. Problematic Stress
Normal stress during pregnancy is temporary and manageable. You worry about a doctor’s appointment. You have a rough day at work. You have a hard workout or presentation. Your body responds, you handle it, and your nervous system returns to baseline. This short-term stress won’t harm your baby.
Problematic stress is chronic, overwhelming, and persistent. Your body stays in “fight-or-flight” mode without relief. Stress hormones stay elevated day after day, week after week.
Pregnancy amplifies how you experience stress. Hormonal changes, particularly progesterone, make your brain more sensitive to stress signals. What felt manageable before pregnancy can feel overwhelming now.
Physical and Emotional Stress Responses
When stress becomes chronic during pregnancy, you might notice:
- Sleep problems (can’t fall asleep, wake up multiple times)
- Persistent headaches or tension
- Changes in appetite
- Racing thoughts that won’t shut off
- Irritability or mood swings
- Physical tension in the shoulders, neck, and jaw
These signals mean your nervous system is stuck in sympathetic dominance—that “go, protect, survive” mode. When you’re in this state, so is your developing baby. Your nervous system is teaching your baby’s developing nervous system what “normal” feels like.
Common Causes of Pregnancy Stress
You’re not stressed because you’re weak. Pregnant women face real, legitimate stressors, often multiple at once. AND how your body was regulating before pregnancy has a big part in it too!
Pregnancy-Related Stressors
- Physical discomforts wear you down. Morning sickness. Exhaustion. Back pain. Heartburn. These aren’t minor when you’re experiencing them day after day.
- Fear about your baby’s health keeps you up at night. Will something go wrong? Every prenatal visit brings anxiety until you hear that heartbeat.
- Fear about labor and delivery is normal. The unknowns are overwhelming. Will you handle the pain? What if you need an emergency C-section?
- Fear about becoming a parent hits hard. Can you do this? How will you manage work and afford everything?
Life Circumstances and External Stressors
- Financial problems create constant worry. Medical bills. Baby gear. Lost income. For many families, financial stress is the biggest burden during pregnancy.
- Work-related stress doesn’t disappear. Meeting deadlines while exhausted. Figuring out maternity leave logistics.
- Relationship difficulties can intensify. Disagreements about parenting. Feeling unsupported. For some women, pregnancy happens during separation or in relationships with domestic violence.
- Health disparities and racism create chronic stress for many pregnant women. Women of color face higher rates of pregnancy complications and often receive dismissive medical care. This systemic stress takes a real toll.
Previous Trauma and Mental Health
- Previous pregnancy loss or miscarriage makes every new pregnancy anxiety-filled. You’re terrified something will go wrong again.
- Fertility struggles and IVF create stress that starts before pregnancy begins. Multiple rounds of treatment, hormones, failures, and financial strain, the nervous system is already depleted before pregnancy starts. This is Stage 1 of The “Perfect Storm.”
- Previous traumatic birth experiences or stories haunt subsequent pregnancies. If your last delivery involved complications or emergency interventions, you’re carrying that trauma.
- Pre-existing anxiety and depression often intensify during pregnancy. The fear of taking medication adds another worry.
- PTSD (Post-Traumatic Stress Disorder) from any source can be triggered during pregnancy. The loss of control over your body and medical procedures can reactivate old trauma responses.
You’re dealing with real stressors you can’t just eliminate. The stress is valid, and it’s affecting both you and your baby.
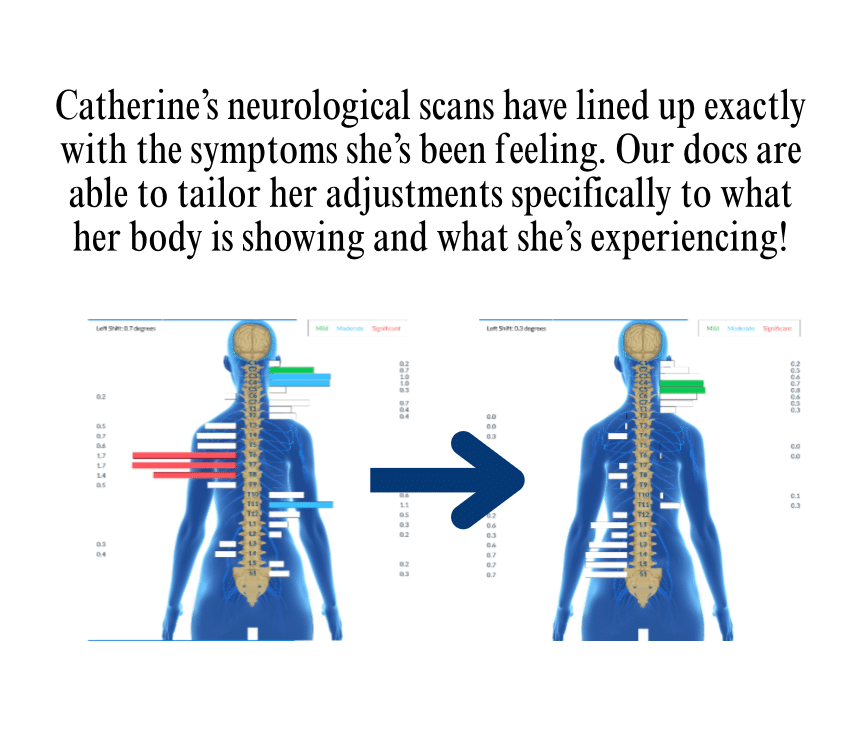
Read this incredible hope story of Catherine and how she overcame prenatal stress and common pregnancy symptoms!

The Physical Impact
Let’s talk about what stress actually does, starting with immediate risks most doctors will tell you about.
Pregnancy Complications Linked to Stress
Research shows chronic stress during pregnancy increases the risk of several complications:
- Preterm birth means delivering before 37 weeks. Studies found that pregnant women with high stress are significantly more likely to go into preterm labor. The mechanism involves CRH (corticotropin-releasing hormone), which triggers labor. When you’re chronically stressed, CRH levels rise, essentially telling your body it’s time to deliver when it’s not.
- Low birth weight often accompanies preterm birth, but can occur in full-term babies too. A low-birthweight baby weighs less than 5 pounds, 8 ounces. Chronic stress affects your baby through the placenta.
- High blood pressure and preeclampsia represent serious complications. Stress activates your sympathetic nervous system, raising blood pressure. Chronic activation increases preeclampsia risk—a condition involving high blood pressure and organ damage.
- Gestational diabetes is connected to chronic stress. Stress hormones affect how your body processes sugar. Cortisol raises blood glucose levels. Constant stress impairs blood sugar regulation.
- Immune system suppression happens when stress hormones stay elevated. Your body deprioritizes immune function for immediate survival, making you more vulnerable to infections.
Stress and Your Baby’s Developing Nervous System
This is where most articles stop. They tell you stress is bad, then move to coping strategies. They’re missing the deeper story.
The Umbilical Cord: More Than Nutrients
That umbilical cord connecting you to your developing baby doesn’t just deliver nutrients and oxygen. It delivers nerve supply. It’s the electrical power cord between your nervous system and your baby’s nervous system.
When you’re stressed, cortisol and other stress hormones cross the placenta. Baby is getting a lot of these stress hormones during the most impressionable period of nervous system development.
How Stress Affects Fetal Brain Development
Research published in Development and Psychopathology tracked pregnant women and their babies. Infants of mothers with the highest stress levels showed 22% higher stress reactivity compared to babies of mothers with the lowest stress. These babies were more easily upset, harder to soothe, and showed poorer recovery.
Here’s what happens in your baby’s developing brain:
The amygdala (fear center) develops larger and more reactive under chronic stress. The HPA axis (your baby’s stress response system) learns its baseline “normal” during pregnancy. If your stress response is constantly activated, your baby’s HPA axis is programmed to match. This creates a hair-trigger stress response that follows them for years.
The Autonomic Nervous System controls heart rate, digestion, breathing, immune function, and sleep. It has two branches: sympathetic (“go, protect, survive”) and parasympathetic (“rest, digest, grow”). When you’re stuck in sympathetic dominance, your baby’s developing nervous system learns this as normal.
Think of it like this: sympathetic is the “gas pedal.” Parasympathetic is the “brake pedal.” Your baby’s nervous system is being built with the gas pedal pressed down and weak brakes.
This is fetal programming.
How Prenatal Stress Creates Lifelong Patterns
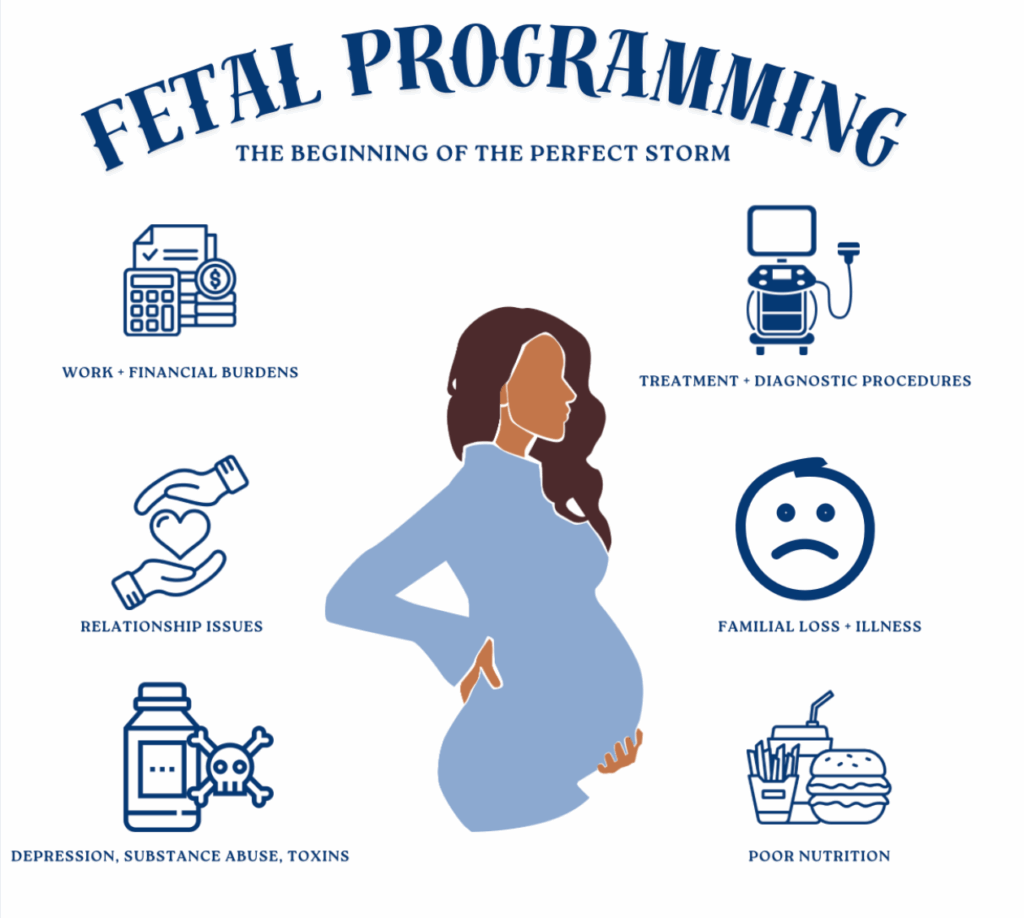
What Is Fetal Programming? At PX Docs, we refer to fetal programming as how events during pregnancy cause permanent structural, physiological, and neurological changes in your developing baby. This isn’t about short-term effects. This is about how your baby’s nervous system, stress response, and even gene expression will function for years.
Pregnancy represents the most critical window. Your baby’s brain will continue developing after birth, but right now is when the foundation gets laid. When basic patterns get established. When programming happens.
Critical Windows and Long-Term Consequences
Your baby’s nervous system is more plastic and moldable right now than it will ever be again. The vagus nerve, the main nerve of the parasympathetic system, is developing its tone and function. When your baby’s nervous system develops in a stressful environment, it adapts to it.
Even after birth, when the environment might be safe, your baby’s nervous system is still programmed for danger. The sympathetic dominance established during fetal programming doesn’t just turn off.
The research on fetal programming and long-term outcomes is extensive:
- Cognitive development: Children of highly stressed mothers have been observed to have a decrease in IQ. This is how prenatal stress affects brain structure.
- Mental health: Kids whose mothers experienced chronic stress during pregnancy have a higher risk of mental health issues. They struggle more with emotional regulation and behavior.
- ADHD and attention problems are more common in children exposed to high prenatal stress. A nervous system programmed for sympathetic dominance can’t focus, can’t settle, can’t regulate attention. It’s constantly scanning for threats.
- Physical health is affected, too. Higher rates of asthma and allergies. More infections. Cardiovascular issues later in life. Even metabolic conditions like obesity and diabetes have roots in fetal programming.
- Sensory Processing Disorder often starts with prenatal stress. When your baby’s nervous system develops in a heightened state, sensory input gets processed differently. The nervous system can’t filter and integrate information properly.
The vagus nerve shows measurable dysfunction in children of stressed mothers. Poor vagal tone means poor regulation of digestion, heart rate, inflammation, immune function, social engagement, and emotional regulation.
Fetal programming explains why some babies seem “difficult” from day one. Some kids struggle with colic, constipation, sleep issues, sensory sensitivities, and behavioral challenges. It’s not bad luck or bad parenting. It’s nervous system dysregulation that started during the most critical window of development.
The “Perfect Storm,” When Pregnancy Stress Is Just the Beginning
At PX Docs, we’ve identified a pattern we call The “Perfect Storm,” a series of stressors during critical developmental windows that create neurological dysfunction.
Prenatal and Fertility Stress
For many families, the “Perfect Storm” begins before pregnancy starts. Fertility struggles. Multiple rounds of IVF. The emotional weight of trying to conceive. Hormonal medications. Financial strain. Relationship stress. Month after month of hope and disappointment.
When pregnancy finally happens, the nervous system is already depleted. Then pregnancy adds its own stressors: fear, physical discomfort, and ongoing anxiety.
Your baby is developing in this environment. The nervous system is being pre-programmed for dysregulation before birth. This is why some babies seem “high needs” from the moment they’re born, their nervous system has learned sympathetic dominance as baseline normal.
The Progression Pattern
The “Perfect Storm” doesn’t stop at birth. It involves birth trauma, interventions, C-sections, forceps, or vacuum extraction. Or early life stressors, antibiotics, ongoing feeding difficulties, and sleep disruption.
Each stage adds stress to a nervous system already dysregulated. You’ve heard doctors say, “Don’t worry, they’ll grow out of it.” But here’s the truth: they don’t grow out of it. They grow into it.
Colic at two months becomes chronic constipation at six months. Constipation becomes sensory sensitivity at 18 months. Sensory issues become ADHD symptoms at age five. ADHD becomes anxiety by age ten.
The nervous system dysfunction that started during fetal programming just manifests differently as the brain develops.
Managing Stress: How We Measure Nervous System Function
Conventional care lacks an objective way to measure its impact on your nervous system. You tell your doctor you’re stressed, but there’s no test or scan. INSiGHT scanning technology changes this.
What INSiGHT Scans Measure
INSiGHT scans provide objective data through three technologies:
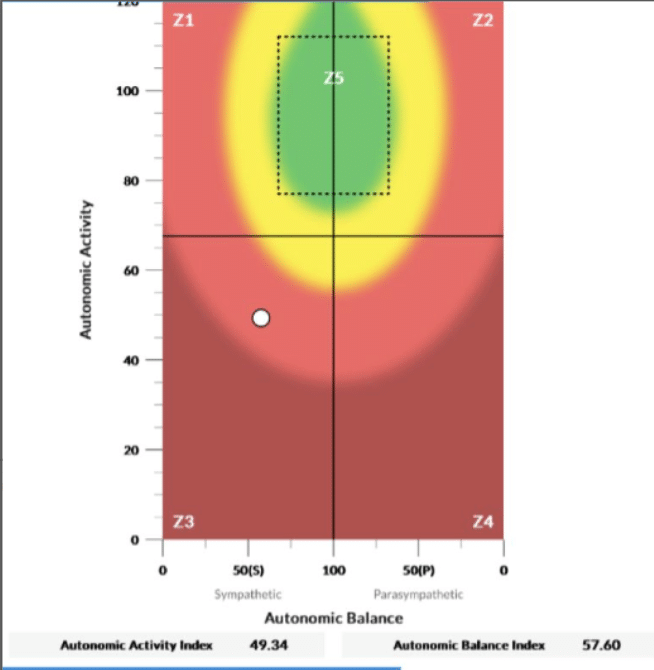
- Heart Rate Variability (HRV) measures the balance between the Sympathetic Nervous System (“fight-or-flight”) and Parasympathetic Nervous System (“rest, regulate, and digest”) branches of the Autonomic Nervous System. When you’re stuck in sympathetic dominance, your HRV shows it. As your nervous system regulates, your HRV improves—often before you notice symptom changes.
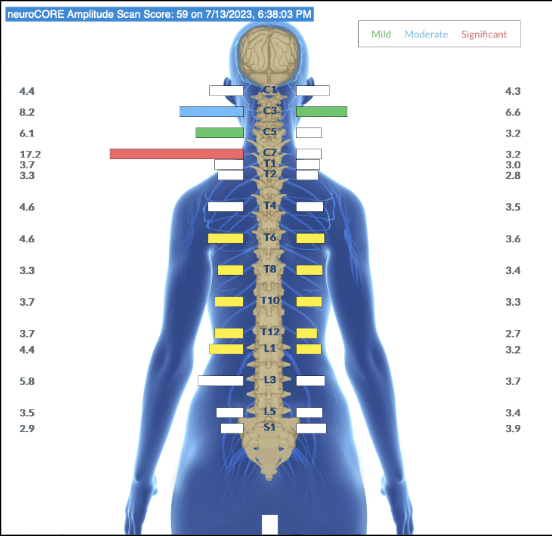
- Surface Electromyography (sEMG) assesses the electrical activity of muscles along the spine, helping to identify areas of tension and altered neuromuscular function or proprioception. This shows where your nervous system is stuck, holding tension. This is also a great scan to show us how the nervous system is communicating with hormones.
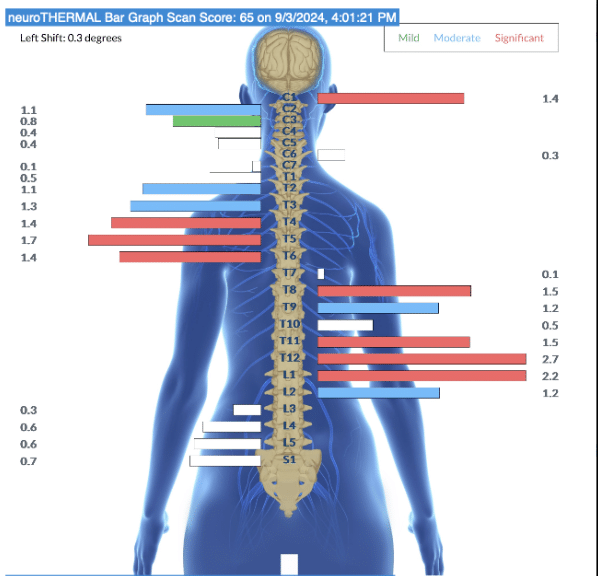
- NeuroThermal scanning uses infrared sensors to measure temperature differences along the spine, which can indicate areas of dysautonomia.
Detecting Changes Before Symptom Improvement
What makes these scans valuable is their ability to detect subtle changes in neurological function long before those changes manifest as trait improvements.
Think of INSiGHT scans like weather radar detecting clear skies forming on the horizon, even if the storm hasn’t fully passed overhead yet. The scans capture improvements in your nervous system regulation before you notice you’re sleeping better or feeling calmer.
For pregnant women, INSiGHT scans provide objective evidence that your nervous system is shifting from sympathetic dominance toward balanced regulation. That shift is exactly what supports optimal fetal programming for your developing baby.
Your Baby’s Nervous System Is Developing Right Now
Your baby’s nervous system is being programmed during this pregnancy. In this moment.
The stress during pregnancy you’re experiencing isn’t just affecting how you feel today. It’s affecting the neurological foundation your baby is building. The patterns being established in your baby’s nervous system during this critical window will influence their health trajectory for years.
But you have more control than you think. Not by eliminating every stressor—that’s impossible. By helping your nervous system regulate despite the stress. By shifting from sympathetic dominance into parasympathetic function. By creating a calm, regulated internal environment that supports healthy fetal programming.
Your nervous system teaches your baby’s nervous system. When you’re regulated, your baby learns regulation.

This is the window of opportunity. Pregnancy is when the foundation gets built. The intervention you pursue now, addressing nervous system dysregulation at the root cause level, affects not just your pregnancy but your child’s lifelong health.
Find a Neurologically-Focused Chiropractor in the PX Docs directory, and learn more about fetal programming. Schedule INSiGHT scans to see where your nervous system needs support. Your child’s healing journey starts here.