When two-and-a-half-year-old Nolan was diagnosed with autism, he struggled with low muscle tone that impacted his gross motor skills. Nolan had great difficulty walking due to hypotonia (low tone) and poor sensory processing, along with limited speech and frequent stimming behaviors.
Though Nolan had been in early intervention therapy for over two years, his mother felt he was stuck and unable to progress. As she shares, despite ongoing therapy, “we felt he was ‘stuck’ and had ‘plateaued’ in progress.” Nolan desperately needed help building core strength, coordination, and regulation skills.
That’s when they found the PX Docs Network, and Nolan began Neurologically-Focused Chiropractic Care, which brought about major breakthroughs for Nolan’s low tone and motor skills. Thanks to intensive neurological chiropractic care, Nolan has gone from struggling to walk to now being able to run – huge strides forward!
If your child with autism struggles with low muscle tone, this article shares Nolan’s story of hope and healing. Discover the impact of low muscle tone, also called low tone, its underlying causes, and most importantly, the effective solutions that are available through Neurologically-Focused Chiropractors within the PX Docs network. There is help available to strengthen your child’s body and nervous system.
What is Autism Spectrum Disorder?
Autism spectrum disorder (ASD) is a complex developmental disability that affects how the brain functions. It impacts how a person communicates, interacts socially, learns, and processes sensory information.
The term “spectrum” refers to the varied severity and combinations of challenges that individuals with ASD can have. No two people have the exact same symptoms. Some children may be nonverbal, while others have fluent speech. Some struggle greatly with sensory overload, while others under-react to stimuli. The presentation varies widely.
While genetic factors play a partial role, research confirms that autism also develops due to environmental factors disrupting nervous system development and function. Things like prenatal stress, birth trauma, gut issues, and toxins converge into what we call the “Perfect Storm” underlying autism.
Symptoms of autism, which can range from mild to very severe, include:
- Delayed speech and language skills
- Difficulty with social communication and interaction
- Repetitive behaviors and restrictive interests
- Sensory processing disorders
- Poor eye contact and reading facial expressions
- Adherence to rigid routines and difficulty with transitions
Autism now affects 1 in 36 children and is over 4 times more prevalent in boys than girls. While there is no medical “cure,” the right interventions can vastly improve nervous system function and quality of life. Let’s explore the role low muscle tone plays.
What is Low Muscle Tone?
Low muscle tone, known medically as hypotonia, refers to decreased muscle strength and reduced resistance or tension in a muscle, even when at rest. Hypotonic muscles have a floppy, loose, or “floppy baby” feel to them.
This low muscle tone makes it more difficult for children to utilize their muscles effectively. Activities like sitting up, crawling, walking, using utensils, and playing sports require extra effort and energy. Low muscle tone can also contribute to poor stability and coordination.
While all babies are born with naturally low muscle tone, it should improve over the first few months of rapid development. When tone remains lower than normal, a child is said to have hypotonia. This low tone is present in various developmental conditions like Down Syndrome, cerebral palsy, and other genetic disorders.
However, functional low muscle tone is also commonly seen in children with autism spectrum disorder. It is estimated that 50% of children with ASD have low tone, compared to much lower rates in the general pediatric population. This points to an important connection between hypotonia and autism.
The technical term for low or weak muscle tone is hypotonia. But you will also frequently hear it referred to more conversationally as “low tone” or “floppy muscles and joints.” Regardless of the terminology, this condition affects muscle strength, motor skills, stability, coordination, and more. Let’s explore further why low muscle tone and autism go hand-in-hand.
Low Muscle Tone and Autism
There is a strong correlation between low muscle tone and autism spectrum disorder.
But why is this connection so common? As we’ve covered, autism is a neurodevelopmental disorder rooted in dysfunction of the central and autonomic nervous systems. This disrupts development in areas like behavior, social skills, speech, and cognition.
Importantly, the nervous system also controls motor development and coordination via nerves that signal our muscles to move and hold positions. When the nervous system is not working properly, it impairs motor tone, leading to the low muscle tone seen in a majority of autistic children.
Low muscle tone in infancy can also contribute to delays in early motor milestones like lifting the head, rolling over, sitting up, crawling, and walking. This puts the child even further behind socially, cognitively, and physically.
In this way, low tone and ASD perpetuate one another—poor nervous system function contributes to low tone, which causes developmental delays and further disrupts nervous system development. That’s why early intervention focused on improving nervous system function is so critical.
Additionally, the sensory processing challenges common in autism make it harder for the child to interpret body positioning and initiate coordinated movements, worsening low muscle tone. Difficulty processing proprioceptive input affects motor planning.
By working to address the root causes, we help children with ASD overcome their low muscle tone, improve developmental milestones, boost nervous system function, and increase their quality of life significantly.
Signs and Symptoms of Low Muscle Tone
How can you tell if your child has low muscle tone that requires intervention? There are several common signs and symptoms to look for:
- Poor posture like rounded shoulders, head tilts forward, slumped sitting position
- Difficulty maintaining upright head control and sitting or standing without support
- Delayed ability to lift head up during tummy time as an infant
- General muscle weakness and poor endurance with fatiguing quickly
- Fluctuating muscle tone that varies throughout the day
- Hypermobile joints that are very flexible
- Difficulty stabilizing joints for movement and coordinating agonist/antagonist muscle groups
- Delays in rolling, sitting, crawling, and walking independently
- Challenges with fine motor skills – holding utensils, writing, buttoning clothes
- Poor control of oral motor muscles – chewing, controlled drooling
- Difficulty integrating both sides of the body together during gross motor activities
Additionally, low muscle tone often contributes to sensory processing disorders, poor proprioceptive awareness, and challenges with motor planning and coordination. Low muscle tone is also often associated with chronic constipation, since movement and motility of the smooth muscles that line the digestive tract are also controlled by the autonomic nervous system.
Caregivers may first suspect low tone in infancy when delays arise in early motor milestones. However, identifying and addressing hypotonia in children as early as possible is ideal to prevent further motor impairments down the road. If you have any concerns about your child’s strength, stability, posture, or motor skills, seeking professional evaluation is recommended.
Causes and Contributing Factors
As with most childhood health conditions today, low muscle tone and developmental delays have complex, multifactorial causes. There is rarely just one reason hypotonia in children develops.
Some common contributing factors include:
- Birth trauma: This includes interventions like c-section delivery, forceps, or vacuum extraction. Physical damage and misalignment (subluxation) of the upper neck and cranium impact nervous system communication and muscle tone regulation.
- Prenatal factors: Exposure to medications, infections, toxins, or maternal stress in utero can impair nervous system development.
- Nervous system dysfunction: Subluxation, inflammation, immune activation, and vagus nerve dysfunction disrupt neural pathways involved in signaling muscles.
- Sensory processing disorders: Difficulty receiving and interpreting proprioceptive input impairs motor control.
- Genetic disorders: Conditions like Down syndrome, Prader-Willi syndrome, and congenital hypotonia also often present with low muscle tone.
- Nutritional factors: Deficiencies in iron, vitamin D, magnesium, or omega-3s may contribute. Poor gut health and food sensitivities also play a role.
Identifying and addressing the root causes, especially subluxation, inflammation, and nervous system dysregulation, empowers the child’s body to strengthen muscle tone naturally.
Impact on Daily Living
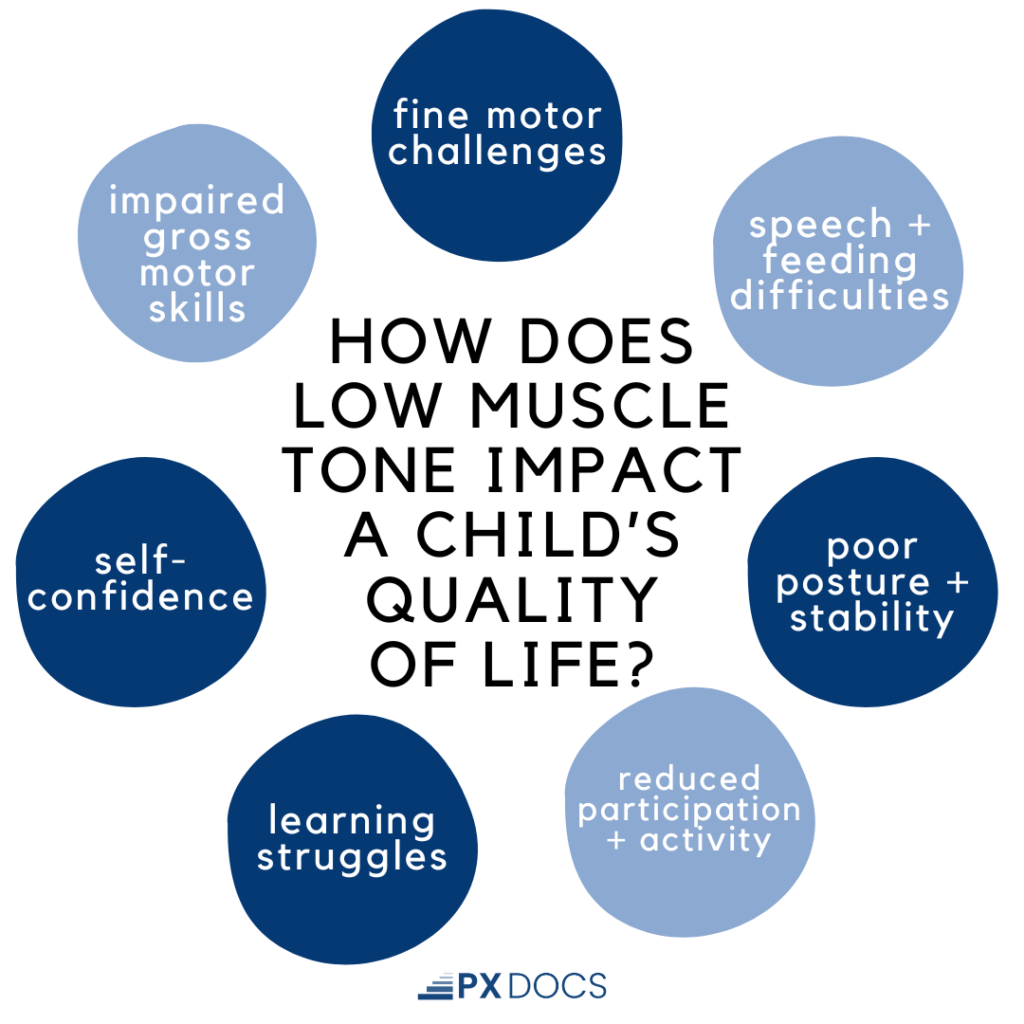
Let’s explore how low muscle tone can impact a child’s daily life and quality of life:
- Impaired gross motor skills: Walking, running, jumping, throwing, catching, kicking balls, and riding bikes require strength and control.
- Fine motor challenges: Using utensils, writing, tying shoes, and buttoning clothes call for precise hand and finger movements.
- Speech and feeding difficulties: Oral motor control is needed for proper chewing, controlled drooling, and clear articulation.
- Poor posture and stability: Sitting upright in class, maintaining head control, and preventing slouching require muscle endurance.
- Reduced participation and activity: Kids avoid sports, playgrounds, camps, and physical education classes because low tone impairs performance and endurance.
- Learning struggles: Weak core and neck muscles make it hard to sit still during lessons and focus. Fatigue sets in quickly.
- Self-confidence: Children realize they cannot perform physical tasks as easily as peers, affecting self-esteem.
The longer low muscle tone goes unaddressed, the wider these developmental gaps become. Kids fall further behind as peers progress. That’s why early intervention focused on nervous system-based solutions is the key to overcoming hypotonia.
Caring for Low Muscle Tone and Autism
While the traditional approach of physical therapy for hypotonia and low muscle tone is one that many families see improvements with, they often occur much slower and with way more time and input needed than would be required if the child’s subluxations and neuromuscular dysfunction were first addressed. Parents whose children are also getting Neurologically-Focused Chiropractic Care often report greatly improved progress with physical therapy, which is a change often noticed and noted by the physical therapist as well.
Many parents see such improvements when adding chiropractic to their child’s care team, that they will intentionally schedule their adjustments just prior to therapy appointments in order to get the maximum result each and every time.
That is the focus of Neurologically-Focused Pediatric Chiropractors within the PX Docs network – optimizing neuromuscular tone, coordination, and function. Our customized care plans help regulate the nervous system, reduce subluxation, decrease inflammation, and stimulate the vagus nerve. This leads to improved communication between the brain and muscles, enhancing motor tone and coordination naturally.
Our gentle adjustments activate key nerves and pathways involved in core strength, stability, posture, and movement. Our doctors are specially trained to detect and correct areas of subluxation through precise Neurological Insight Scans and drug-free care protocols.
As mentioned above, our PX Docs also look to work in coordination and collaboration with a child’s physical, occupational, and speech therapy team, working to ensure optimal outcomes for each and every patient.
The key difference in our approach is that it addresses the underlying neurological causes of hypotonia rather than just looking to work on the muscles and soft tissues. This is how children regain optimal function and reach their full potential. We see it happen every day through empowering families with the tools and care options they need.
A Child’s Nervous System Holds the Key
Low muscle tone in children with autism is an extremely common challenge that affects quality of life and functional abilities significantly. The first step would be to work with a neurologically focused chiropractor to identify areas of subluxation, neurological interference, and vagus nerve dysfunction through advanced scans and high-quality care protocols. Support your child’s body in building strength naturally.
Consistency is key – just like learning to walk, developing muscle tone and coordination takes steady practice. But you will be amazed at the strides your child makes when their nervous system can communicate with the body properly.
There is hope and help available. To find a PX Doc trained and ready to help in your area, check out our PX Docs directory today. Your child’s future starts now.





