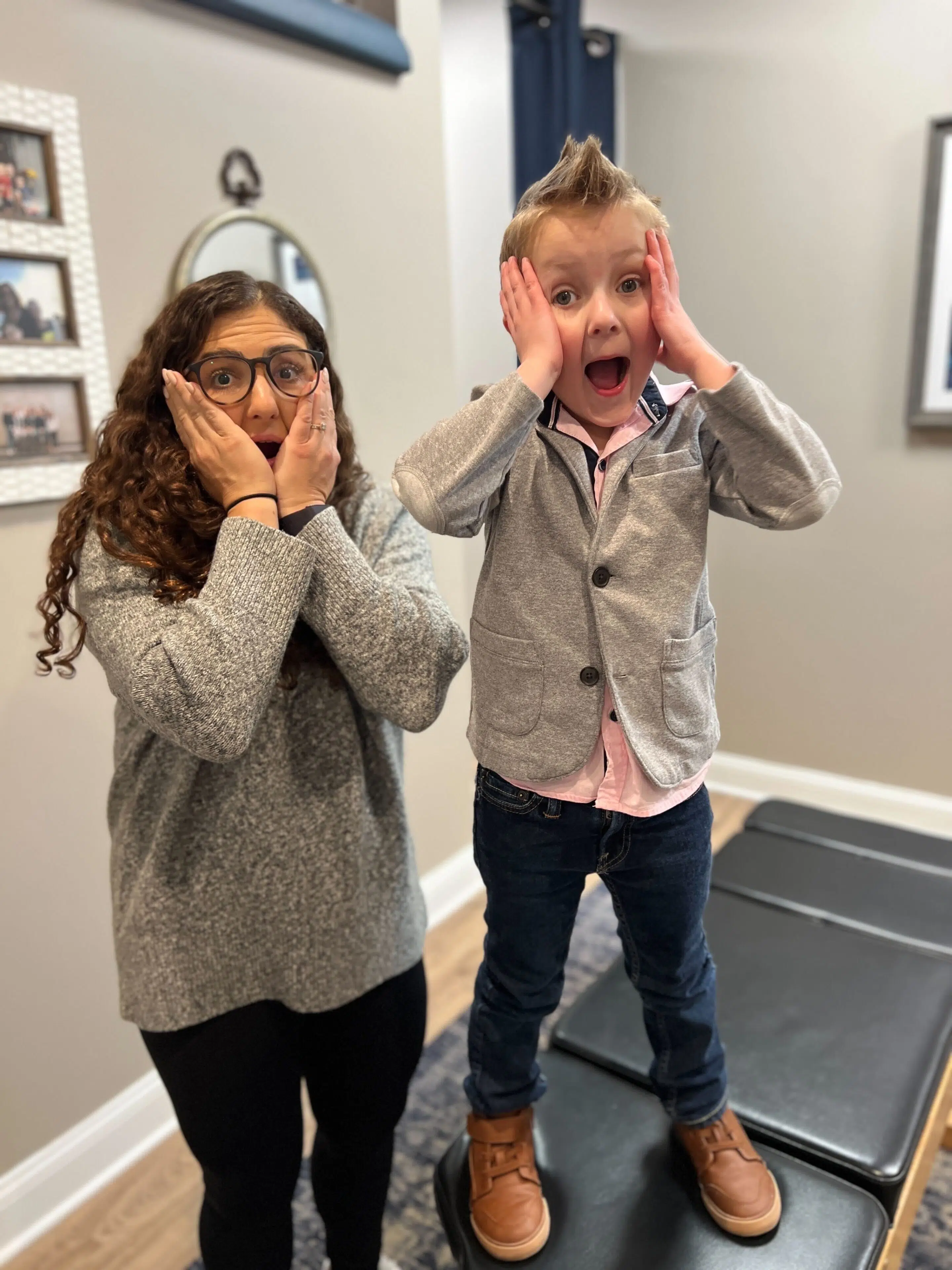
“You were speaking our language as no one else has before. We felt heard and like someone else understood our challenges for the first time.”
Those were the words a dad shared with me during our consultation all the way back 10+ years ago, when I wrote my very first article on Sensory Integration Disorders for a local magazine.
Not only had they met very few practitioners at that time who had even heard of Sensory Integration Disorder, but they also really understood that it was a significant challenge that negatively affected the quality of life of their child day in and day out.
Thankfully, we could give these parents and this child more explanation and information on what was causing the Sensory Integration Disorder challenges in their son. We also created a very thorough action and care plan designed to vastly improve their quality of life by addressing the sensory issues at their root.
What Are Sensory Integration Disorders?
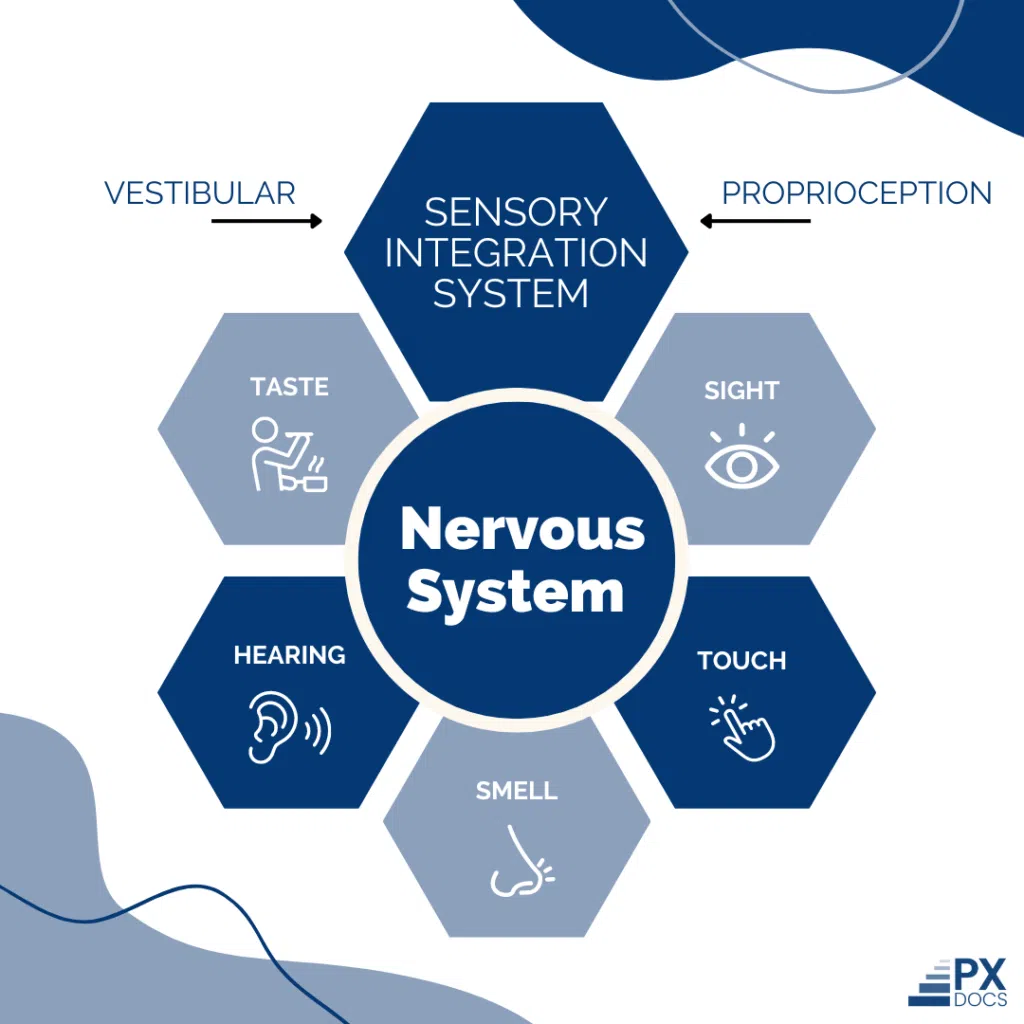
The nervous system is responsible for receiving and processing sensory information, and this process is more formally known as sensory integration. Sensory Integration Disorders (SID), also often referred to as Sensory Processing Disorders (SPD), are conditions in which the brain struggles to properly process sensory stimulation.
Research shows that at least 1 in 20 children (5%) experience sensory processing difficulties significant enough to impact daily life.
Dr. A. Jean Ayres, a pioneering occupational therapist and neuroscientist who researched sensory integration throughout the 1960s and 1970s, developed the foundational theory that still guides most occupational therapy approaches today. She suggests that sensory conditions like these are similar to a “neurological traffic jam” that ultimately prevents sensory information from being processed and sent where it needs to go. This can affect how children (and adults) regulate behavior, perform motor functions, and go about many other day-to-day activities.
When we say sensory information, we mean anything our bodies detect with one of our senses, like taste, touch, smell, hearing, and sight. There are also three “internal” senses that specialists associate with body awareness (proprioception), movement (vestibular), and internal body states (interoception).
The central nervous system, particularly the brainstem and thalamus, must receive, interpret, and integrate sensory input from all these systems simultaneously for your child to function smoothly in their environment.
One tricky element of Sensory Processing Disorders is that everyone can be affected differently. Some people are overstimulated, and even the most common noises or lightest touches can be uncomfortable or even painful. On the other hand, some people struggle to fully understand or sense stimulation, potentially making them uncoordinated or spatially unaware.
Sensory integration and learning conditions are usually identified during childhood, but they can be identified in adults as well. Note that the traditional medical industry currently doesn’t view Sensory Integration Disorders as a legitimate diagnosis; instead, medical professionals often relate the signs to other conditions.
Understanding the Core Sensory Systems
To understand Sensory Processing Disorder, you need to know about the three primary sensory systems that form the foundation of how your child experiences and responds to the world.
The tactile system includes sensory receptors under the skin that send information about touch, pressure, pain, and temperature to the brain. When this system is dysfunctional, you’ll see tactile defensiveness—your child refuses to touch certain textures, can’t stand tags in clothes, won’t get their hands messy, or experiences light touch as painful. Some kids go the opposite direction, constantly seeking tactile input by touching everything.
Here’s where the “Perfect Storm” connection becomes clear: birth trauma and early nervous system stress can create hypersensitivity in the tactile system. The vagus nerve, which processes sensory information from the skin and plays a major role in how we perceive touch, can become dysregulated during the birth process or through accumulated stress in early childhood.
The vestibular system, located in the inner ear, detects head movement, changes in position, and helps maintain balance and spatial awareness. This system tells your child where they are in space and provides what’s called “gravitational security.” When dysfunctional, some children develop gravitational insecurity—terrified of playground equipment, fearful of heights, getting motion sickness easily. Others show the opposite pattern—constantly seeking vestibular input through spinning, jumping, and climbing.
The vestibular system is particularly vulnerable during birth. Forceps, vacuum extraction, and the pulling and twisting that happens during delivery can disrupt the delicate inner ear structures and the upper cervical spine that houses these critical balance centers.
Think of the vestibular system as helping your child’s nervous system know when to hit the gas pedal (activate and engage) or the brake pedal (calm down and regulate). When this system isn’t working right, your child’s nervous system gets stuck with the gas pedal pressed down—constantly seeking more input—or the brake pedal jammed—fearful and avoiding movement altogether.
The proprioceptive system uses receptors in muscles, joints, and tendons to provide subconscious awareness of body position and movement. When proprioceptive dysfunction exists, children appear clumsy, constantly bump into things, don’t understand their own strength, and may develop Postural Disorder. Many children with Sensory Processing Disorder crave proprioceptive input—they love crashing, jumping, and “heavy work” activities because this input helps their nervous system feel organized and regulated.
Over-Responsive vs. Under-Responsive
Children can be over-responsive (sensory-avoiding) or under-responsive (sensory-seeking) to stimulation. Some children show a mix of both patterns, depending on which sensory system is involved.
Over-responsive children may struggle with clothes that are too itchy, sounds that are too loud, lights that are too bright, screaming when touched, gagging at food textures, poor balance or clumsiness, poor motor skills, and behavioral problems like meltdowns or extreme resistance to everyday activities.
Under-responsive children often engage in sensory-seeking behaviors: trouble sitting still, don’t pick up on social cues or personal space, thrill-seeking behaviors, don’t get dizzy while spinning, don’t respond to extreme temperatures, want constant visual stimulation, chew on things, have a high pain threshold, and don’t always understand their own strength.
These signs often significantly affect motor skills. Children may struggle with fine motor skills like holding a pencil or buttoning clothing. Gross motor skills challenges include difficulty climbing stairs, catching a ball, or riding a bike. Many children also exhibit bilateral coordination problems—difficulty using both sides of the body together.
Physical signs often lead to secondary behavioral challenges. When children can’t process sensory stimulation effectively, they may experience frequent meltdowns, poor self-esteem, social isolation, and mental health struggles like anxiety and depression. What appears to be “bad behavior” is often a child’s nervous system in survival mode, overwhelmed by sensory input they can’t regulate.
Try our Sensory Processing Disorder test to see if this may be the case for your child.
How Sensory Processing Disorder Affects Daily Life
Getting dressed becomes a 45-minute battle. Meals are stressful; your child survives on 5-7 “safe” foods while everyone else worries about nutrition. At school, the classroom lights seem too bright, the noise level overwhelming, and sitting still feels impossible. Teachers label them as “difficult” or “attention-seeking” when really their nervous system is drowning in sensory input.
Birthday parties and playdates end in meltdowns. The chaos, noise, and unexpected touches from other children create sensory overload that looks like “bad behavior” to others who don’t understand. You find yourself declining invitations, watching your child become increasingly isolated.
When sensory processing difficulties disrupt daily living to this degree, both child and family suffer. Everyday activities that others take for granted become exhausting challenges that leave everyone stressed and frustrated.
The “Perfect Storm”: Understanding Root Causes
The “Perfect Storm” often begins before birth. Maternal stress—whether physical, emotional, or chemical—floods the developing baby’s nervous system with stress hormones. This doesn’t make mothers responsible; rather, it reveals how vulnerable the developing central nervous system is during critical formation periods.
Then comes birth. While medical interventions save lives, they also create physical stress on the infant’s nervous system. Forceps delivery and vacuum extraction can apply 110-150N of traction force to a newborn’s head and neck. Even scheduled C-sections require a significant pulling force. This trauma particularly affects the upper cervical spine and brainstem, where the vestibular system and vagus nerve reside.
The very structures responsible for processing sensory input get compressed, twisted, and misaligned during delivery. What conventional medicine calls a “normal” birth can create lasting neurological dysfunction in these critical sensory processing areas.
The third stage happens in early childhood. A baby with unaddressed birth trauma often experiences colic, reflux, and sleep difficulties—all signs of dysautonomia. They may receive multiple rounds of antibiotics for ear infections, which can disrupt gut health and immune function. Each stressor compounds on a nervous system already struggling to regulate. By age 3-7, the accumulated stress can manifest as full Sensory Processing Disorder, ADHD, anxiety, or developmental delays.
The role of subluxation—characterized by spinal fixation and resulting nervous system dysfunction—is often overlooked. When the upper cervical spine becomes misaligned during birth or early childhood, it creates interference in neural pathways between the body’s sensory receptors and the brain’s processing centers.
Is Sensory Processing Disorder a “Real” Diagnosis?
Here’s a frustration many parents face: Sensory Processing Disorder isn’t recognized in the DSM-5 (the official psychiatric diagnostic manual). The American Academy of Pediatrics recommended in 2012 that pediatricians not use SPD as a standalone medical diagnosis. Many insurance carriers won’t cover sensory integration therapy because it lacks official diagnosis codes.
You know your child. When everyday activities become daily battles, when your child melts down from stimuli others barely notice, when social isolation develops because birthday parties are overwhelming—this is real. The absence of a DSM-5 code doesn’t change your child’s experience or your family’s stress.
What matters more than the diagnostic label is understanding what’s causing your child’s sensory processing difficulties and finding effective solutions. This is where looking at root causes rather than trait categories becomes critical for your child’s healing.
Are SID/SPD Signs of Autism?
Research suggests up to 97% of individuals with Autism Spectrum Disorder also experience sensory processing difficulties. However, many—potentially most—people with SPD don’t have Autism.
While there’s overlap in sensory signs, the underlying neurodevelopmental differences are distinct. SPD specifically involves how the brain processes sensory information—the “neurological traffic jam” that prevents smooth integration of sensory input. Autism involves broader differences in social communication, behavioral patterns, and cognitive processing that extend well beyond sensory issues alone.
Pediatric chiropractors trained in Neurologically-Focused care assess and address these conditions as separate concerns with distinct nervous system patterns. Through INSiGHT scanning technology, we can identify the specific neurological dysfunction patterns present—whether they align with Autism, SPD, or both—and create customized care plans accordingly.
Conventional Care Approaches
Occupational therapy remains the most common conventional care. Occupational therapists specializing in sensory integration therapy use play-based activities in controlled environments. In a sensory gym, children might swing for vestibular input, crash into mats for proprioceptive feedback, or explore various textures for tactile system regulation.
A “sensory diet”—a customized schedule of sensory activities—helps children stay regulated throughout the day. This might include weighted blankets, fidget tools, movement breaks, heavy work activities, noise-canceling headphones, or designated calm-down spaces.
Occupational therapy provides tremendous value—it teaches children coping strategies and helps them tolerate challenging sensory input. Many families see initial improvements that genuinely change their daily lives.
However, many families notice a plateau after 6-12 months. Children improve their coping skills, but the underlying sensitivity remains. They can tolerate tags in clothing, but it still bothers them. They’ve learned to compensate for nervous system dysfunction rather than resolving it.
This is because conventional sensory integration therapy focuses on teaching the brain to adapt to dysfunctional sensory processing. It’s trait management—helping your child function better despite ongoing neurological dysfunction. The therapy works on the behavioral response to sensory challenges, but doesn’t address what created the sensory processing difficulties in the first place.
Neurologically-Focused Chiropractic Care for Sensory Integration Disorders
While teaching kids how to regulate and exposing them to different scenarios can be part of an overall strategy, addressing the underlying neurological dysfunction offers a different path. PX Docs and appropriately trained pediatric chiropractors focus on the root cause: subluxation and dysautonomia affecting the central nervous system.
When the upper cervical spine—particularly where the brainstem, vestibular system, and vagus nerve reside—experiences fixation from birth trauma or early childhood stress, it creates interference in sensory processing at the neurological level. Addressing this subluxation removes the interference, allowing the nervous system to process sensory information more effectively. Instead of teaching your child to cope with dysfunctional processing, we’re working to restore normal processing function.
PX Docs uses INSiGHT Scanning Technology. These computerized scans objectively measure nervous system dysfunction, dysautonomia, and stress patterns in just 10-15 minutes. The scans reveal exactly where neurological interference exists—often in the upper cervical spine where sensory integration centers connect.
What makes INSiGHT scans powerful is that they provide objective measurements of nervous system function before signs fully improve. Parents often see the scans shift toward normal patterns weeks before behavioral or sensory traits resolve—proof that the nervous system is healing from the inside out.
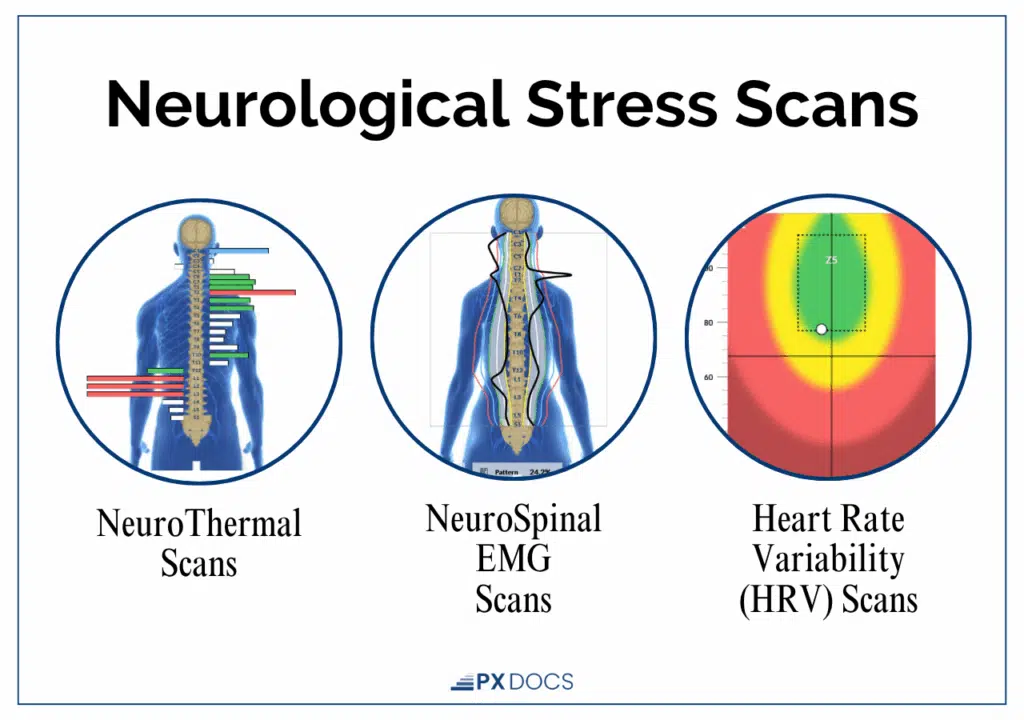
After the scan, our trained PX Docs can create a customized care plan that includes adjustments focusing on sensory, motor, and other neurological benefits. The goal isn’t to suppress sensory responses or teach better coping—it’s to restore normal nervous system function so your child can naturally process sensory input the way they were designed to.
Discover a Simple Solution For Sensory Integration Disorder
If your child struggles daily with sensory challenges, know that there is hope beyond managing the signs. With the right understanding and care—especially care that looks at the root causes within the nervous system—your child can find calm, focus, and comfort again. You don’t have to navigate this alone. Visit our PX Docs directory to connect with a trained pediatric chiropractor near you and take the first step toward lasting relief and a brighter, more balanced future for your child.