Oliver just couldn’t catch a break. For the third time that year, his little body was racked with that distinctive, scary barking cough that signaled yet another bout of croup. As a premature birth who had faced significant respiratory challenges at birth, including a six-week NICU stay, Oliver was at high risk for croup and other breathing difficulties. His parents felt helpless listening to him struggle.
If you’ve ever heard the telltale seal-like cough of croup, you understand how frightening it can be. Croup affects about 3% of children in the U.S. each year, with peak incidence in toddlers around 2 years of age. While it’s usually not serious, croup can lead to severe breathing difficulties in some little ones.
As a parent, understanding what causes croup, recognizing the signs, and knowing your care options—both at home and in partnership with your child’s healthcare providers—is crucial. No one wants to see their child struggling to breathe. By equipping yourself with knowledge about this common childhood ailment, you can help your child weather the croup storm and emerge thriving.
What is Croup?
Croup is a common respiratory illness that causes swelling and inflammation in the upper airways, particularly the larynx (voice box) and windpipe (trachea). This swelling leads to a characteristic barking cough and can make breathing difficult, especially for young children.
There are three main types of croup:
- Viral Croup: The most common type, usually starting as a typical cold but progressing to inflammation in the voice box and barking cough. A low-grade fever may also accompany it.
- Spasmodic Croup: Often comes on suddenly, typically at night, and may be triggered by allergies or reflux. The barking cough is present, but there is usually no fever.
- Croup with Stridor: This condition occurs when the airway swelling is severe enough to cause a high-pitched squeaking sound (stridor) when inhaling. It can indicate more serious breathing difficulties.
Croup most commonly affects children between 6 months and 3 years old, with peak incidence around 2 years old. According to the American Academy of Pediatrics, croup accounts for about 15% of pediatric respiratory illnesses yearly.
Younger children are more susceptible to croup because their airways are smaller and their immune systems more immature. Infants born prematurely or those with asthma or other respiratory conditions may experience more severe symptoms. As children grow, their airways expand, making croup less common after age 5.
Children who are prescribed antibiotics early in life, which are commonly misused and overused, also are likely to be more susceptible to other types of infections, including croup cough since they disrupt their delicate microbiome and neuro-immune function.
While croup can be scary for both children and parents, it is typically manageable at home. However, it’s crucial to recognize the signs of more severe breathing difficulties that require immediate medical attention.
Signs and Symptoms of Croup
Recognizing the symptoms of croup is essential for parents to know when their child needs extra care and support. The hallmark sign of croup is the distinctive chronic cough, but there are several other symptoms to watch for:
- Barking Cough: The most telltale croup symptom is a loud, harsh cough that sounds like a seal barking. This cough is often worse at night and can be triggered by crying or agitation.
- Stridor: In more severe cases, children may make a high-pitched squeaking noise when breathing in, called stridor. This sound indicates significant swelling in the upper airways.
- Difficulty Breathing: Children with croup may experience labored breathing, rapid breathing, or retractions (when the skin between the ribs pulls in with each breath). This can be frightening for both children and parents.
- Fever: Viral croup is often accompanied by a low-grade fever, typically under 102°F (38.9°C).
- Hoarseness: Your child’s voice may sound hoarse or muffled due to inflammation in the larynx.
Other symptoms of croup can include:
- Runny nose or congestion
- Decreased appetite
- General fussiness or irritability
Similar to Respiratory syncytial virus, or RSV, croup symptoms often start like a typical cold, then suddenly worsen at night. The barking cough and noisy breathing can be alarming, but try to stay calm. Comforting your child and helping them rest can prevent further agitation that may worsen symptoms.
In milder cases of croup, symptoms usually improve within 3-5 days. However, if your child is struggling to breathe, has stridor (high-pitched breathing) at rest, or can’t speak or swallow, seek emergency medical care right away. We’ll discuss when to go to the hospital later in this article.
Causes of Croup Cough
While croup can be alarming for parents, understanding its causes can help you better support your child’s health and reduce their risk of severe episodes. The most common cause of croup is a viral infection. Most commonly, these include:
- Parainfluenza viruses
- RSV
- Influenza viruses
- Adenoviruses
- Enteroviruses
These viruses are highly contagious and can spread easily through respiratory droplets when an infected person coughs or sneezes, or by touching contaminated surfaces and then touching the face or mouth. Children are particularly susceptible to these viruses because their immune systems are still developing.
“The Perfect Storm” of Risk Factors
In addition to viral infections, several other factors can come together to create “The Perfect Storm” of increased risk for croup and other respiratory illnesses in children:
- Stress During Pregnancy: Maternal stress during pregnancy can impact the developing nervous system of the fetus, potentially increasing the risk of nervous system dysfunction and croup later in life.
- Birth Interventions: Procedures like C-sections, forceps, and vacuum extraction can cause physical stress and trauma to an infant’s delicate spine and nervous system, leading to subluxation and dysautonomia that may contribute to croup susceptibility.
- Nervous System Dysfunction: Subluxation and dysautonomia can disrupt the normal functioning of the nervous system, making it harder for children to regulate their immune responses and increasing their vulnerability to infections like croup.
- Underdeveloped Immune System: Infants and young children have immature immune systems that are still learning to recognize and fight off infections, which can make them more prone to viral illnesses like croup.
- Early Exposure to Antibiotics: Even when used appropriately, these medications can disrupt the delicate balance of the still-developing microbiome and neuro-immune system, leaving a child more susceptible to respiratory illnesses like croup later in life.
Other Croup Cough Triggers
In some cases, croup episodes may be triggered by factors other than viral infections, such as:
- Allergies or Reflux: These conditions can cause inflammation and irritation in the upper airways, leading to spasmodic croup symptoms.
- Growth Spurts: Rapid growth can sometimes trigger croup episodes, as the body’s resources are directed towards development, potentially impacting immune function.
- Seasonal Changes: Croup cases often increase during the fall and winter months when cold and flu viruses are more prevalent.
By understanding the various factors that can contribute to croup, parents can take steps to support their child’s overall health and immunity, such as reducing stress, supporting nervous system function through chiropractic care, and practicing good hygiene to limit virus exposure.
How Children with Croup Cough Are Often Diagnosed
If you suspect your child has croup, it’s essential to have them evaluated by a healthcare provider. Doctors can typically diagnose croup based on a physical examination and a review of the child’s symptoms and medical history.
During the examination, your doctor will:
- Listen to your child’s breathing for the characteristic barking cough and stridor
- Check for signs of respiratory distress, such as trouble breathing or skin retractions
- Assess your child’s overall appearance and level of comfort
- Look for other signs of illness, like fever or congestion
In most cases, additional tests are not needed to diagnose croup. However, if your child’s symptoms are severe or not improving with treatment, your doctor may recommend:
- Pulse oximetry to measure blood oxygen levels
- Neck or chest X-rays to rule out other conditions or check for complications
While PX Doctors and Pediatric Chiropractors are licensed to evaluate and diagnose, this is where we take a similar but also significantly different approach than medical providers. Our analysis and care approach is much more focused on identifying the root cause and neurophysiological dysfunction leading to the symptoms of croup, rather than diagnosing and treating it (stuffing down symptoms and covering them up).
Our adjustments seek to boost and support the body’s own natural defenses and neuro-immune function, opening up the airway by releasing stuck tension and constriction, boosting vagal nerve tone and parasympathetic function (calming, regulating), and addressing unwanted neurological interference and inflammation.
When to Seek Emergency Care for Croup Cough
While most cases of croup can be managed at home, it’s crucial to know when your child needs immediate medical attention. Seek emergency care if your child:
- Has trouble breathing or cannot speak due to breathing difficulties
- Has stridor (high-pitched breathing sounds) at rest
- Develops a bluish tint around the mouth, indicating low oxygen levels
- Becomes extremely agitated or lethargic
- Shows signs of dehydration, such as dry mouth, sunken eyes, or decreased urination and begins to refuse liquids
- Has a fever higher than 102°F (38.9°C) or a fever lasting more than three days
If you’re ever unsure whether your child’s symptoms warrant emergency care, it’s always best to err on the side of caution and have them evaluated by a medical professional. Which is another reason why it is so valuable to have a PX Doctor on your healthcare team. Not only can their care help support the body naturally, but they can evaluate your child alongside you and support you in the medical decision-making process.
Home Care for Croup Cough
For mild cases of croup, home care measures can help soothe your child’s symptoms and promote recovery. Here are some tips:
- Prioritize rest: Encourage your child to get plenty of sleep and avoid overexertion, as rest helps the body heal.
- Maintain hydration: Offer frequent sips of water, clear broth, or other clear fluids to prevent dehydration. Popsicles can soothe sore throats from barking cough.
- Create a soothing environment: Use a cool-mist humidifier or have your child breathe in steam from a hot shower to help moisten the airways and ease breathing. You can also try taking them outside for a few minutes to breathe in the cool night air, which can sometimes help reduce swelling.
- Natural Remedies: Certain natural remedies like essential oils, vitamins, supplements, and homeopathic remedies can help strengthen the body and its own natural defenses.
- Offer comfort: Soothe your child with gentle back rubs, cuddling, or reading stories. Keeping them calm and comfortable can prevent further irritation of the airways.
Remember, if your child’s symptoms worsen or they develop difficulty breathing, seek medical care right away.
Conventional Medical Interventions for Croup
For more severe cases of croup, medical interventions may be necessary to help reduce inflammation and open the airways. The most common treatments include:
- Corticosteroids: Oral or injectable steroids like dexamethasone can help reduce swelling in the larynx and trachea, making breathing easier. A single dose is often effective, but some children may need a short course of treatment.
- Epinephrine: In the hospital setting, nebulized epinephrine (adrenaline) may be given to quickly reduce airway swelling in severe cases. The effects are temporary, so close monitoring is essential.
- Oxygen therapy: If your child’s oxygen levels are low, supplemental oxygen may be provided to support breathing.
While these treatments can be lifesaving in severe cases, it’s important to note that they do carry some risks. Corticosteroids and epinephrine can have side effects like increased blood pressure, agitation, and impaired immune function over time. That’s why it’s crucial to use these interventions judiciously and to focus on natural prevention strategies whenever possible.
Some ways to support your child’s immune system and reduce the risk of croup include:
- Encouraging a nutrient-rich, whole-food diet
- Ensuring adequate sleep and stress management
- Staying physically active and spending plenty of time outdoors as a family
- Adding in supportive vitamins, supplements, and minerals
- Supporting nervous system function through regular chiropractic care
By taking a proactive, holistic approach to your child’s health, you can help them build resilience and weather illness more easily.
The PX Docs’ Approach to Croup Cough
At PX Docs, we recognize that true health comes from within. While conventional medical care plays a vital role in managing severe illness, we believe that addressing the underlying nervous system dysfunction is key to building long-term resilience and vitality.
As the master control system of the body, the nervous system regulates all functions, including immunity, digestion, and respiratory health. When subluxation and dysautonomia are present, it can lead to a cascade of health challenges, including increased susceptibility to conditions like croup due to the role sympathetic dominance plays in creating respiratory constriction, inflammation, and immune system dysregulation.
Subluxation, which involves dysfunction and nervous system interference, can disrupt normal communication between the brain and body. This can lead to dysautonomia, or an imbalance in the autonomic nervous system, causing the “fight or flight” sympathetic response to become dominant. Over time, this can weaken the immune system, increase inflammation, and make it harder for the body to heal.
How Neurologically-Focused Chiropractic Care Can Help With Croup Cough
Pediatric chiropractic care identifies and addresses subluxation and nervous system dysfunction through specific adjustments. By restoring nervous system function, chiropractic can help:
- Reduce dysregulation and inflammation by promoting balance between the sympathetic and parasympathetic nervous systems
- Enhance respiratory function by releasing tension in the neck, chest, and diaphragm muscles
- Improve sleep, digestion, and overall resilience by supporting the body’s natural healing capacity
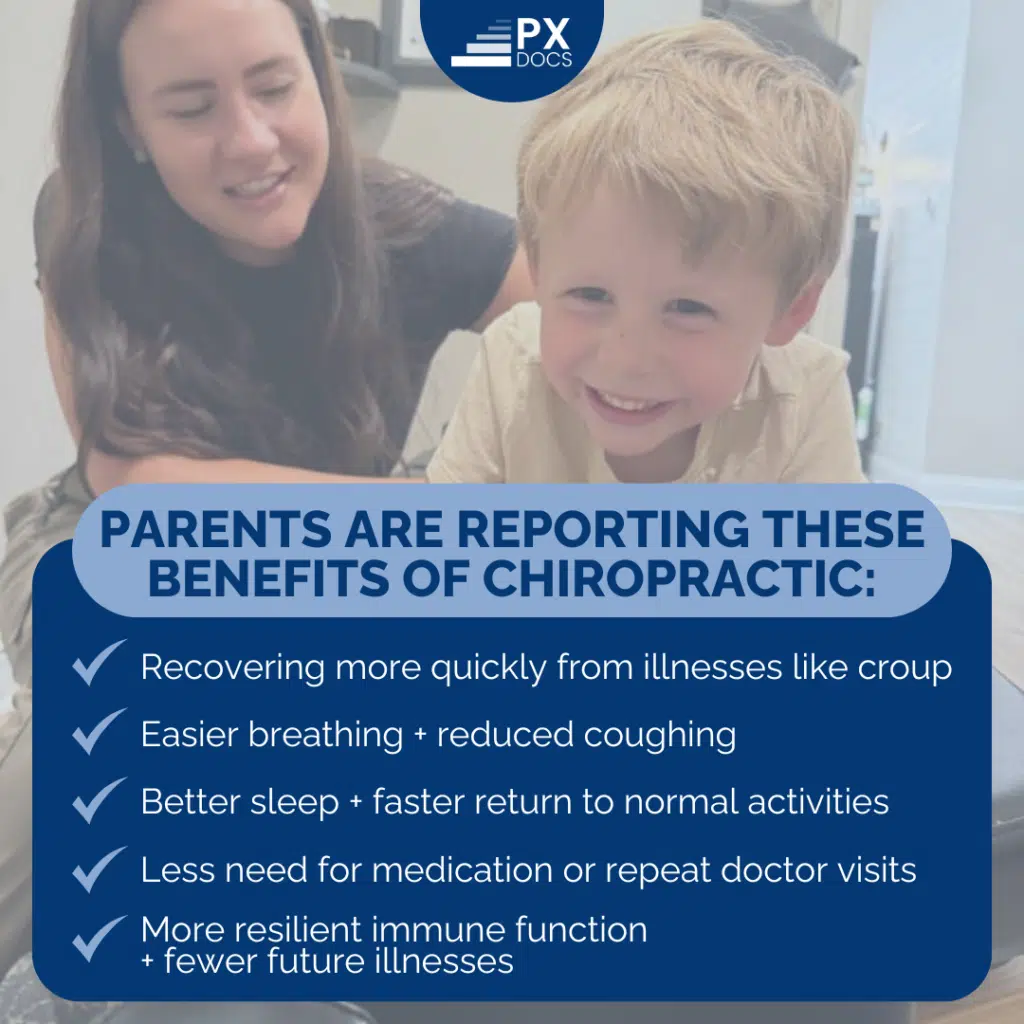
Many parents report that regular chiropractic care helps their children recover more quickly from illnesses like croup, with benefits like:
- Easier breathing and reduced coughing
- Better sleep and faster return to normal activities
- Less need for medication or repeat doctor visits
- More resilient immune function and fewer future illnesses
At PX Docs, we use advanced technology like INSiGHT Scans to precisely identify areas of nervous system stress and tailor our care to each child’s unique needs. By addressing the root cause of dysfunction, rather than simply managing symptoms, we help children build a foundation for lifelong health and well-being.
Empowered Care for Healthier Kids with Croup Cough
As a parent, you are your child’s greatest advocate and ally. When faced with concerns like a croup cough, it’s natural to feel worried or even helpless. But by educating yourself and partnering with trusted healthcare providers, you can navigate these challenges with confidence and compassion.
Remember, most cases of croup are manageable at home with simple measures like rest, hydration, and creating a soothing environment. For extra support, get your child in for extra supportive boost adjustments to help them fight off these challenges naturally and drug-free.
Trust your instincts—if your child is struggling to breathe or showing signs of severe illness, don’t hesitate to seek emergency care.
For ongoing support and preventive care, consider adding a qualified PX Doctor to your child’s wellness team. By addressing the underlying nervous system dysfunction that can contribute to conditions like croup, Pediatric Chiropractic Care can help your child build resilience and thrive. Visit our directory to find a PX Doc near you and take the first step towards empowered health.