Kylie was dealing with a relentless cycle of congestion, a perpetually runny nose, and seasonal allergies. Her parents were determined to find a solution to alleviate her suffering. They explored countless drug-free protocols and experimented with various supplements, which provided some relief, but it felt like a crucial piece of the puzzle was missing.
What are Seasonal Allergies?
Watching her struggle with extreme seasonal allergies was tough, so Kylie’s parents were determined to uncover the missing link that would help them reach the root cause. Little did they know that their journey to understanding her struggles would open their eyes to a whole new world of seasonal allergy management.
Seasonal allergies, also known as hay fever or allergic rhinitis, are allergic reactions that occur during specific times of the year. They are triggered by environmental factors such as pollen from trees, grasses, and weeds. While anyone can develop seasonal allergies, children are at a higher risk since their immune system is still developing.
Seasonal allergies (also called allergic rhinitis) affect approximately 24 million Americans, including 1 in 4 children, making it one of the most common chronic conditions. Unlike perennial allergies that occur year-round from triggers like dust mites, seasonal allergies follow predictable patterns tied to plant pollination cycles.
Unfortunately, kids today are at greater risk of seasonal allergies than ever before due to the decline in their overall health. The increase in rates of obesity, inflammatory conditions, and even neurodevelopmental challenges in kids today all play a role in increasing their struggles with seasonal allergies and related symptoms.
Repeated exposure to allergens, such as pollen, is necessary for the immune system to develop a hypersensitivity response. This means that after multiple encounters with a specific allergen, such as birch tree pollen, the body’s immune system mistakenly perceives it as a threat. As a result, the immune system releases antibodies that attack the allergens within the pollen, triggering the release of histamines in the blood.
Signs and Symptoms of Seasonal Allergies
Recognizing allergy symptoms in children is important so parents can determine whether their child is dealing with a common cold, an ear infection, or truly suffering from seasonal allergies.
We encourage parents to keep an eye out for the following symptoms:
- Sneezing: Frequent, repetitive sneezing, especially during specific times of year, may indicate seasonal allergies.
- Itchy, Watery Eyes: Persistent itching and watery eyes are hallmark allergy symptoms that distinguish them from colds.
- Runny or Stuffy Nose: Persistent itching or a constantly runny nose, even without a cold, can be a sign of allergies.
- Nasal Congestion: Difficulty breathing through the nose due to nasal congestion is a common symptom of seasonal allergies.
- Scratchy Throat: An itchy or scratchy throat can accompany other allergy symptoms in children.
- Postnasal Drip: The sensation of mucus dripping down the back of the throat can be indicative of allergies.
- Fatigue: Seasonal allergies can cause fatigue and a general feeling of low energy.
- Poor Concentration: Allergy symptoms can impact a child’s ability to concentrate and focus on daily activities.
- Increase in Ear and Sinus Infections: Seasonal allergies may make children more prone to ear and sinus infections.
Unlike cold symptoms that resolve in 7-10 days, allergy symptoms persist for 6+ weeks during pollen season, as long as allergens remain in the air. If you notice these symptoms occurring around the same time each year, your child is likely affected by seasonal allergies.
If that’s the case, you’ll want to use the resources in this article to address their root cause directly, deploying natural solutions to strengthen your child’s neuro-immune system so that over time, they can experience fewer allergy symptoms and a more enjoyable quality of life during those seasons.
Causes of Seasonal Allergies
While traditional medicine still views the primary cause of seasonal allergies as mere exposure to pollen and certain allergens, the answer to what causes the symptoms and health challenges lies in immune system dysfunction.
If we continue to view the pollen or allergens themselves as the primary problem, then avoiding them by staying indoors during the most beautiful and enjoyable times of the year will greatly limit the quality of life for kids and individuals with seasonal allergies.
While it’s totally normal for everyone, especially children with developing immune systems, to get a bit of a stuffy nose or chest congestion during seasonal shifts and times of high pollen counts, it’s not normal to develop seasonal allergies.
In individuals with allergies, the immune system overreacts, mistaking pollen as dangerous and triggering an allergic inflammatory response. When the immune system identifies an allergen, it produces histamines as a defense mechanism.
When allergens trigger immune cells, they release histamines, leukotrienes, and prostaglandins—inflammatory chemicals that cause itching, swelling, and increased mucus production. The vagus nerve normally regulates this inflammatory cascade. When nervous system dysfunction occurs, this regulatory control weakens, leading to exaggerated allergic responses.
Histamines are responsible for the typical allergy symptoms such as sneezing, itchy or runny nose, nasal congestion, scratchy throat, postnasal drip, fatigue, poor concentration, and an increased susceptibility to ear and sinus infections.
Seasonal Allergy Calendar
While most seasonal allergy sufferers struggle in both spring and fall, there are key differences depending on what they are most allergic to.
Spring Allergies (March-May)
Tree pollen kicks off spring allergies, as dormant trees come alive and release pollen into the air from March through May in most regions. Common allergenic trees include:
- Birch (one of the most common offenders in northern latitudes)
- Oak, maple, ash, and elm
- Cedar, alder, willow, and poplar
Tree pollen counts are typically highest in the evening hours. Warm days and cool nights create ideal conditions for pollen release. Unfortunately, pollen can trigger an allergic response in kids and people with dysfunctional immune systems and neurological imbalances.
Summer Allergies (May-July)
Grass pollen season overlaps with late spring and extends through summer (May-July). The most common grass allergens include:
- Ryegrass and timothy grass
- Bluegrass, orchard grass, and sweet vernal grass
- Bermuda grass (in warmer southern climates)
According to the Asthma and Allergy Foundation of America, grasses are the most common seasonal allergy trigger.
Fall Allergies (August-November)
In the fall, ragweed pollen, released primarily from August to November, is a common source of allergy symptoms during that season. Ragweed pollen can travel hundreds of miles on windy days, affecting even those who don’t live near ragweed plants.
Typically, ragweed pollen counts are highest in mid-September and peak in the morning hours, especially on dry, windy days. Ragweed pollen season ends with the first hard freeze, providing relief by November in most northern regions.
Mold is also a typical trigger for fall allergies, as it thrives in moist, damp environments. The rotting leaves of fall provide a perfect home for mold growth, which releases mold spores into the air. These tiny spores can cause nasal congestion, runny noses, sneezing, and watery, itchy eyes for those who struggle with seasonal allergies.
Winter (December-February)
Most outdoor allergens lie dormant during winter, bringing relief to many with seasonal allergies. However, spending more time indoors means increased exposure to indoor allergens like:
- Dust mites (in bedding, carpets, upholstery)
- Pet dander (cat and dog proteins)
- Mold spores (in damp areas like bathrooms, basements)
- Cockroach allergens
Children with nervous system dysfunction may react to both seasonal and indoor allergens, explaining why symptoms never fully resolve.
The Neurological Connection to Seasonal Allergies
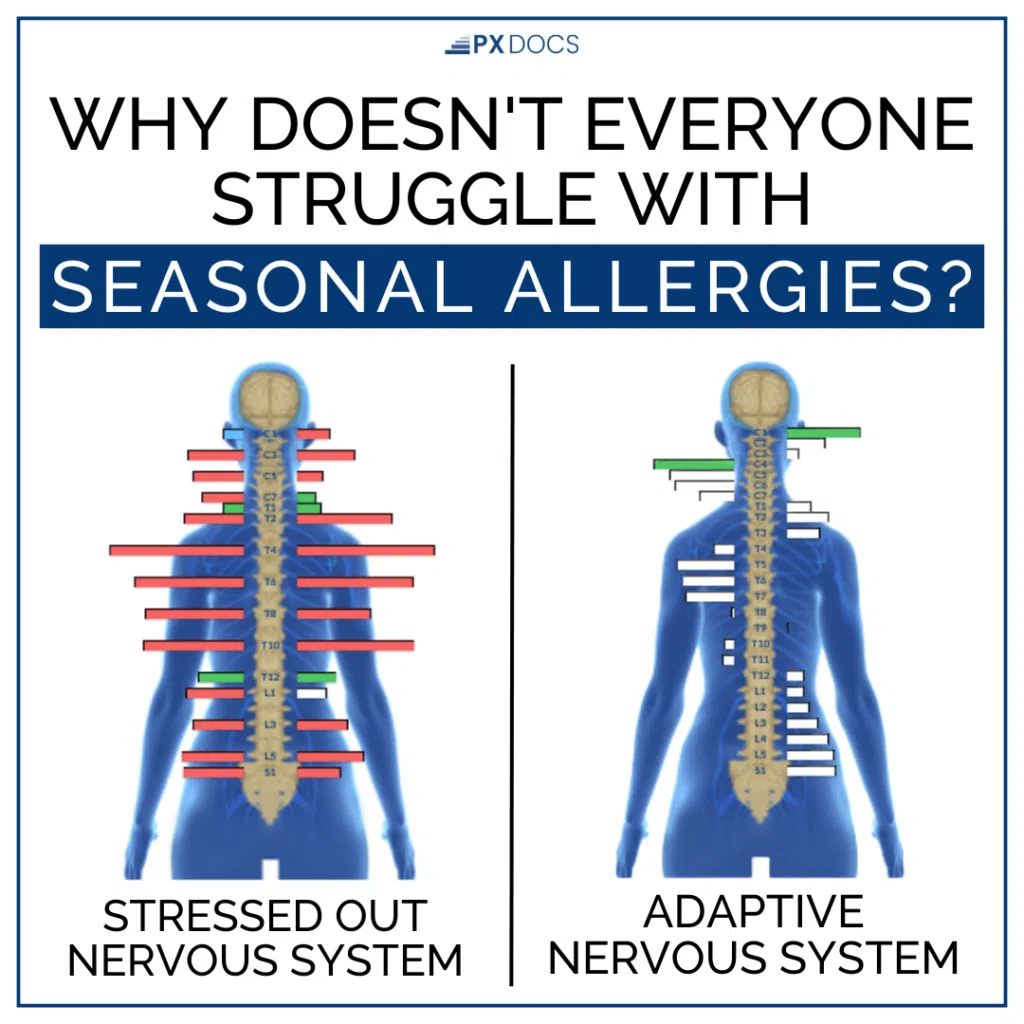
The number one thing that makes our work as PX Docs different is that we keep digging until we reach the real root cause, rather than just focusing on the symptoms of a condition. So, in the case of seasonal allergies, we need to determine what is causing the underlying immune system dysfunction and hypersensitivity.
This is where the allergy conversation needs to shift from focusing only on the immune system to instead focusing on the connection between the nervous and immune systems.
While most natural health experts point to toxins and other pro-inflammatory elements of the environment, such as gluten and dairy, as additional factors here, we must also consider the role that increased exposure to stress and altered neurological development plays.
A crucial, easily overlooked component that may contribute to the development of seasonal allergies in kids is that the Central and Autonomic Nervous Systems must properly develop first for the immune system to function appropriately. Meaning, for many children, the real root cause of their allergy symptoms and immune system hypersensitivity is often an overstressed and imbalanced nervous system.
This dysfunction and imbalance of the nervous system is called subluxation, a complex neurological dysfunction characterized by three components:
- Dysfunction within the neurospinal system
- Fixation and restricted movement (decreased proprioception)
- Neurological interference that disrupts communication between the brain and body.
The Gut-Immune-Nervous System Connection
Understanding allergies requires seeing the full picture. Research suggests that approximately 70-80% of immune cells reside in or originate from gut-associated lymphoid tissue (GALT), and gut barrier function is regulated by the vagus nerve.
Here’s how it works: nervous system dysfunction → poor vagal tone → gut barrier dysfunction → immune hypersensitivity.
When the gut barrier becomes compromised, allergens trigger stronger immune reactions. Bacterial dysbiosis (imbalanced gut bacteria) intensifies this inflammatory response.
If the nervous system is like the master control panel in a manufacturing plant, the gut is the production floor where immune cells are made. When the control panel malfunctions, say from birth trauma or chronic stress, the production floor gets bad instructions. It starts producing too many inflammatory chemicals, overreacting to harmless pollen as if it were a dangerous invader.
The “Perfect Storm”
This is where the “Perfect Storm” concept becomes clear.
Birth trauma (C-section, forceps, vacuum extraction) can damage the delicate vagus nerve. Early antibiotic use disrupts gut bacterial balance. Chronic stress keeps the nervous system in a state of sympathetic overdrive. None of these alone may cause severe allergies, but the accumulation creates a “Perfect Storm” of immune hypersensitivity.
If the core neurological dysfunction, a condition known as dysautonomia, is not also directly addressed, the child’s immune system will remain in a pro-inflammatory, hypersensitive state at all times, continually overreacting to common things like pollen and other allergens.
When the Sympathetic Nervous System is stuck in overdrive and overstimulated, which is the most common presentation for kids with dysautonomia and subluxation, excessive stress hormones like cortisol are produced.
It’s like your gas pedal (sympathetic system) is stuck down, but your brake pedal (Parasympathetic Nervous System) isn’t working. The car’s still got gas, but you can’t slow down, and that’s when the immune system goes haywire with allergies. This weakens the immune system and allows an excessive inflammatory response to be triggered more easily.
How To Avoid Allergy Triggers
- Monitor Pollen Counts Daily: Check local pollen levels in weather reports, apps, or on the National Allergy Bureau website (pollen.aaaai.org). Keep children indoors during peak pollen hours (morning for ragweed, evening for trees and grasses) when counts exceed 9.7 (high level).
- Control Indoor Air Quality: Use air conditioning with HEPA filters (high-efficiency particulate air) rather than opening windows during pollen season. Consider placing portable HEPA air purifiers in children’s bedrooms for cleaner air during sleep. Change filters every 3-6 months for optimal effectiveness.
- Natural Symptom Relief: Nasal irrigation with saline solution using a neti pot or squeeze bottle rinses pollen and other allergens directly from nasal passages. This drug-free approach can reduce allergy symptoms significantly.
- SAFETY CRITICAL: Use only distilled, sterile, or previously boiled and cooled water. Tap water can contain microorganisms that cause serious infections.
- Reduce Indoor Allergen Exposure: Indoor allergens can trigger symptoms year-round or worsen seasonal allergies:
- Wash bedding weekly in hot water (130°F minimum)
- Use allergen-proof covers on mattresses and pillows
- Remove carpets and upholstered furniture when possible
- Maintain humidity levels between 30-50% using a dehumidifier
- Fix water leaks promptly to prevent mold growth
- Keep pets out of bedrooms
- Vacuum with a HEPA filter twice weekly
While taking measures like staying indoors, keeping the windows closed, cleaning HVAC filters, tracking pollen levels, and taking immune system suppressing medications are the most common things allergy sufferers are told to do, good health does not come from avoiding things, but rather from overcoming them.
By the time we meet most of our allergy patients and they’re ready to give natural health solutions a try, they’ve not only exhausted all over-the-counter and even prescription medical options, but they’re exhausted and tired of the restrictions on their quality of life as well.
That is why taking the neurologically-focused and natural health approach that we guide our patients through as PX Docs is so exciting for those struggling with seasonal allergies! Not only is this a new path and approach for them to address the root cause head-on, but our care options, unlike allergy medications, are free of unwanted side effects and instead improve their health and resiliency in many other ways as well.
Raising Healthy Kids Naturally Playbook
This guide is perfect for individuals and families seeking to build a strong foundation for a drug-free, healthy life.
When to Seek Professional Help
Consider consulting a healthcare provider if your child’s allergy symptoms:
- Interfere with sleep, school performance, or daily activities
- Don’t improve with over-the-counter medications after 2-3 weeks
- Include breathing difficulties, wheezing, or chest tightness
- Lead to frequent sinus infections or ear infections
- Occur alongside suspected asthma
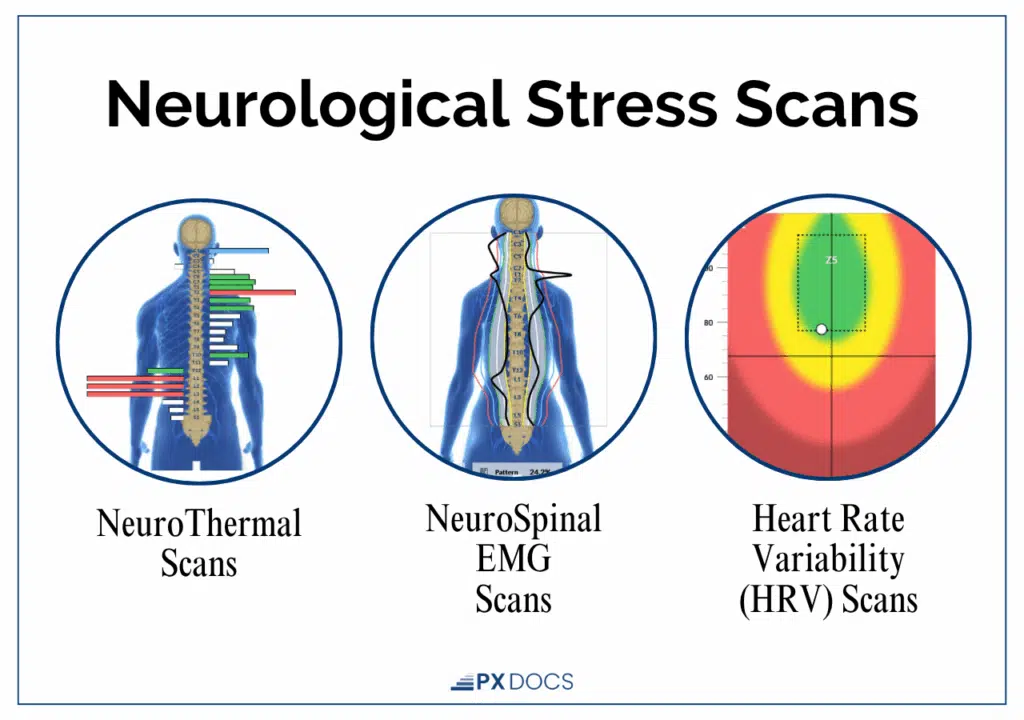
If conventional approaches haven’t provided lasting relief, or if you’re seeking to address root causes rather than manage symptoms, a neurologically-focused assessment using INSiGHT Scans can reveal underlying nervous system dysfunction driving immune hypersensitivity.
Natural Health Options for Seasonal Allergies
When it comes to addressing seasonal allergies, Neurologically-Focused Chiropractic Care seeks to address the neurological and immune system dysfunction head-on.
Our PX Docs Care Plans seek to restore balance to the Autonomic Nervous System, activating and stimulating the vagus nerve and Parasympathetic Nervous System so that, in turn, we can decrease the overactive and overstressed Sympathetic Nervous System that is so often “stuck on” in patients struggling with seasonal allergies.
Neurologically-Focused Chiropractic Care does not seek to treat or cure seasonal allergies but instead works to rebuild and restore optimal neurological and immune system function. By identifying and addressing any disturbances that may hinder the body’s optimal functioning, our care can support the immune system in maintaining balance and lead to a more accurate and efficient response to allergens.
This natural and Neurologically-Focused approach to caring for seasonal allergies not only addresses the root cause but also helps kids and families avoid the unwanted side effects of allergy medications. Common side effects of these medications include drowsiness, fatigue, and constipation, but they can also lead to increased behavior and emotional dysregulation problems since they stimulate an already overstimulated Sympathetic Nervous System.
When Kylie came into a PX Doc office for care, her INSiGHT Scans revealed stress and tension in her body, which was negatively affecting her nasal passages and immune system’s functionality. However, with the introduction of gentle chiropractic adjustments, the accumulated tension and stress began to dissipate, providing her body the opportunity to clear out her sinuses effectively.
Through consistent chiropractic care, Kylie experienced improvements in her overall well-being, especially newfound relief from allergies and chronic sinus issues. Her runny nose disappeared, and she was even able to reduce her dependence on supplements. The transformation allowed Kylie to embrace life fully, enjoy warm weather, and play outdoors with her friends and brother, all while feeling internally and externally content and healthy.
Get Help Today
Seasonal allergies can disrupt the joy of outdoor activities and everyday life for children. Fortunately, with the right care and guidance, it is possible to overcome these immune system dysfunctions and imbalances, and help your child enjoy the changing seasons without discomfort and constant congestion!At PX Docs, our experts specialize in providing comprehensive care for children with seasonal allergies. If your child is struggling with seasonal allergies, don’t hesitate to find a PX Doc near you and discover the relief they deserve.