As a parent, you’ve likely faced a situation where your child has a bacterial infection, and your pediatrician prescribes antibiotics. In fact, approximately 20% of all pediatric outpatient visits result in an antibiotic prescription, with amoxicillin being the most commonly prescribed, used over 50 million times per year in the United States. While these powerful medications can be lifesaving, understanding how long amoxicillin stays in your child’s system is crucial for ensuring proper care and minimizing side effects.
After your child’s last dose of amoxicillin, the medication is primarily excreted through the kidneys over 6-8 hours. By the 12-hour mark, amoxicillin becomes undetectable in the bloodstream. However, while the drug clears quickly, its effects on gut bacteria, immune function, and nervous system regulation can persist much longer, especially in young children during critical developmental windows.
The reality is that antibiotics are often overprescribed for viral infections or mild conditions that would typically resolve on their own. But there’s an even deeper question most parents don’t think to ask: Why does my child keep needing antibiotics in the first place?
Antibiotics are drugs designed to either stop bacteria from reproducing or destroy them altogether. They work against bacterial infections but are ineffective against viral infections, such as the common cold or flu. Understanding how long the medication remains active in your child’s body helps ensure proper care, minimizes side effects, and reduces the risk of antibiotic resistance. More importantly, it helps you understand how repeated antibiotic courses may be affecting your child’s developing nervous system and long-term health.
What are Antibiotics?
Antibiotics are medications used to treat bacterial infections by either killing bacteria or preventing them from multiplying. As broad-spectrum antibiotics, medications like amoxicillin work against many types of bacteria rather than targeting just one specific pathogen.
The discovery of antibiotics in the early 20th century revolutionized medicine, saving countless lives and transforming the care of bacterial infections. Before antibiotics, even simple infections could be deadly, and surgery carried a high risk of complications due to infection. Today, antibiotics are among the most commonly prescribed medications, particularly in children.
Common conditions treated by antibiotics in children include:
- Strep throat
- Urinary tract infections
- Bacterial pneumonia
- Skin infections
- Lyme disease.
Antibiotics are effective against bacterial infections, but their overuse can lead to the development of antibiotic-resistant bacteria. Research shows that without further policy action, drug-resistant infections could claim over 39 million lives by 2050. That’s why it’s essential to use antibiotics only when necessary and as prescribed by a healthcare provider.
Types of Antibiotics and Their Mechanisms
There are several different classes of antibiotics, each with its own mechanism of action. The most common classes prescribed for children include:
- Penicillins (e.g., amoxicillin): These penicillin-type antibiotics work through cell wall synthesis inhibition, causing bacteria to rupture and die. This bactericidal action means they actively kill bacteria rather than just stopping their growth.
- Cephalosporins (e.g., cefdinir, cephalexin): Like penicillins, these beta-lactam antibiotics also interfere with bacterial cell wall synthesis.
- Macrolides (e.g., azithromycin, clarithromycin): This class inhibits bacterial protein synthesis, preventing bacteria from growing and multiplying.
- Tetracyclines and Fluoroquinolones: These work by inhibiting bacterial protein synthesis or DNA synthesis, respectively.
Antibiotics can also be classified as either bactericidal or bacteriostatic. Bactericidal antibiotics, such as penicillins and cephalosporins, kill bacteria directly, while bacteriostatic antibiotics, like tetracyclines, prevent bacteria from growing and reproducing, allowing the body’s immune system to eliminate the infection.
Understanding the specific type of antibiotic prescribed for your child is essential, as different classes of antibiotics can have varying durations of action in the body. This, in turn, can affect how long the medication remains in your child’s system and the potential for side effects or interactions with other substances. Always discuss the specific antibiotic with your child’s healthcare provider and follow their instructions carefully to ensure the best possible outcome.
How Long Does Amoxicillin Specifically Stay in Your Child’s System?
If you’re asking “how long does amoxicillin stay in your system,” here’s what you need to know: After your child’s last dose, the medication begins clearing rapidly through the kidneys. Amoxicillin has a relatively short half-life of approximately 61.3 minutes—meaning the concentration in your child’s bloodstream reduces by half in this timeframe. Within 8 hours, approximately 60% has been eliminated through the kidneys and urine. By the 12-hour mark, amoxicillin levels become undetectable in the blood.
The pharmacokinetics of amoxicillin, which refers to how the drug moves through your child’s body, involve quick absorption, distribution, and excretion. Its bioavailability ranges from 74% to 92%, meaning most of what your child takes gets absorbed and used. Amoxicillin reaches peak plasma concentration within 1-2 hours after ingestion, when it’s working at maximum effectiveness.
Because amoxicillin is primarily excreted through the kidneys via renal clearance, kidney function plays the most critical role in elimination speed.
Why Finishing the Full Course Matters
It’s critical to complete the full course of amoxicillin as prescribed, even if your child feels better. If you stop early, within 6-8 hours, the bacteria could start multiplying again, potentially developing drug-resistant bacteria that make future infections much harder to treat. Your prescription is designed to maintain effective drug levels long enough to completely eliminate the infection.
Factors That Affect How Long Amoxicillin Stays in Your Child’s System
While the standard elimination timeline is 6-8 hours, several factors can significantly affect duration:
- Kidney Function: The most important factor. Children with compromised kidney function may take several days to clear amoxicillin. Healthcare providers typically order dosage adjustments to prevent medication buildup.
- Age and Developmental Stage: Newborns (0-3 months) have immature kidney function and may take 24+ hours for complete elimination. Most children and adolescents generally clear within 6-8 hours.
- Body Weight: Affects both prescribed dosage (calculated as mg/kg) and clearance rate.
- Hydration Levels: Adequate hydration supports kidney function and speeds elimination. Dehydration can slow clearance and increase side effects.
- Overall Health and Metabolism: Fever, illness severity, and individual metabolic differences all influence elimination. Some children naturally metabolize medications faster than others.
- Nervous System Regulation: Your child’s nervous system regulation directly affects medication absorption and processing. The nervous system controls digestive function, including gastric emptying and intestinal motility. Children with nervous system dysregulation often experience digestive issues that affect medication effectiveness.
Potential Side Effects and Risks of Antibiotics
While generally safe when used appropriately, antibiotics can cause side effects, including digestive issues, allergic reactions, yeast infections, and fatigue.
One of the most significant concerns is the impact on the gut microbiome. Gut microbiota disruption extends far beyond digestive upset—it can affect immune function, mood regulation, behavior, and brain development. These effects can persist for weeks or months after the antibiotic clears, especially during critical developmental windows (ages 0-3 years).
Signs of Allergic Reactions to Watch For
Because amoxicillin is a penicillin-type antibiotic, children with penicillin allergies often react to amoxicillin too.
- Immediate reactions (within 1 hour): Hives, facial swelling, difficulty breathing, throat tightness, rapid heartbeat
- Delayed reactions (5-10 days): Widespread rash, itching, fever, joint pain
- Severe reactions: Blistering skin, severe diarrhea (potentially bloody), severe stomach cramps, unusual bruising, yellowing of skin or eyes
Stop medication immediately and seek emergency care for immediate reactions. Contact your healthcare provider if you experience delayed reactions.
Managing Common Side Effects
- Nausea: Give with food to reduce gastrointestinal discomfort
- Diarrhea: Ensure hydration; consider probiotics 2-3 hours apart from doses
- Taste disturbances: Use plastic utensils, offer cold foods, mask flavor with cheese or applesauce
- Yeast infections: Watch for oral thrush or diaper rash
Studies show that less than one-third of antibiotics prescribed in pediatric settings were necessary, contributing to resistance and unnecessary side effects.
Why Does My Child Keep Needing Antibiotics? Understanding Root Causes
If your child has been prescribed amoxicillin multiple times this year, you’re not alone. Many parents face a frustrating cycle of repeated infections and antibiotic courses.
Here’s what most pediatricians miss: They care for each infection individually without asking why your child is so susceptible to infections in the first place. The reality is that some children are “antibiotic kids,” while others rarely need antibiotics. The difference isn’t luck or exposure, it’s neurological.
The “Perfect Storm:” Why Some Children Need Antibiotics Repeatedly
At PX Docs, we’ve identified the “Perfect Storm,” three critical factors that create chronic infection susceptibility:
1. Prenatal Stress: Maternal stress during pregnancy crosses the placenta and impacts fetal development, potentially compromising immune system formation from the beginning. Prenatal stress comes from work pressure, relationship stress, financial concerns, or pregnancy anxieties, helping explain why some children start life with dysregulated nervous systems.
2. Birth Trauma: Birth trauma is the most overlooked factor in childhood health challenges. Physical stress from C-sections, vacuum extraction, forceps, prolonged labor, or even “normal” deliveries affects the baby’s delicate upper cervical spine and nervous system.
The upper cervical spine houses pathways for cranial drainage. When subluxation—neurological dysfunction—is present, it limits the “plumbing,” preventing mucus and fluid from draining properly from the ears, nose, throat, and respiratory tract. This creates an environment where bacteria thrive, leading to recurrent infections.
3. Early Life Stressors: First antibiotic courses in infancy, gut microbiome disruption during critical windows (ages 0-3), daycare exposures, sleep disruption, and dietary challenges compound existing dysregulation.
This creates a vicious cycle: Birth trauma → Subluxation → Poor drainage → Infections → Antibiotics → Disrupted gut bacteria → Weakened immunity → More infections → More antibiotics.
The Dysautonomia Connection
Dysautonomia, Autonomic Nervous System dysfunction, ties these factors together. When stuck in sympathetic “fight-or-flight” mode rather than balanced with parasympathetic “rest-and-digest” function, the immune system doesn’t function optimally, drainage systems don’t work efficiently, and the body can’t mount strong natural responses to infections.
This explains why some children “catch everything” while siblings stay healthy despite identical exposures. It’s not about exposure—it’s about nervous system capacity to respond.
The PX Docs Perspective
At PX Docs, we focus on root cause, natural, drug-free care solutions. We do not cure conditions. However, our approach addresses the neurological dysfunction that weakens immunity and creates conditions for frequent infections.
How Neurologically-Focused Chiropractic Care Addresses Root Causes
We’re not focused on bones and alignment—we’re focused on nervous system function. Neurologically-focused chiropractic care targets subluxation—neurological dysfunction interfering with proper nervous system signaling. Using precise, gentle pediatric adjustments, we work to remove interference and allow proper function.
When subluxation is addressed, drainage improves. The “plumbing” of the ears, sinuses, and respiratory tract begins working properly. Mucus and fluid drain naturally. The environment changes, not because we’re killing bacteria, but because we’re restoring the body’s natural capacity to maintain health.
The vagus nerve, the longest cranial nerve running from the brainstem through the neck into the body, plays a critical role in immune function. When vagus nerve dysfunction is present due to upper cervical subluxation, the immune system doesn’t receive proper signals. Addressing subluxation helps restore vagal tone and support optimal immune function.
The Role of INSiGHT Scans
We use INSiGHT scans, advanced neurological technology, to objectively measure nervous system function. This includes:
- NeuroThermal scanning (autonomic imbalance)
- Surface EMG (muscle tension patterns)
- Heart Rate Variability (sympathetic vs. parasympathetic balance).
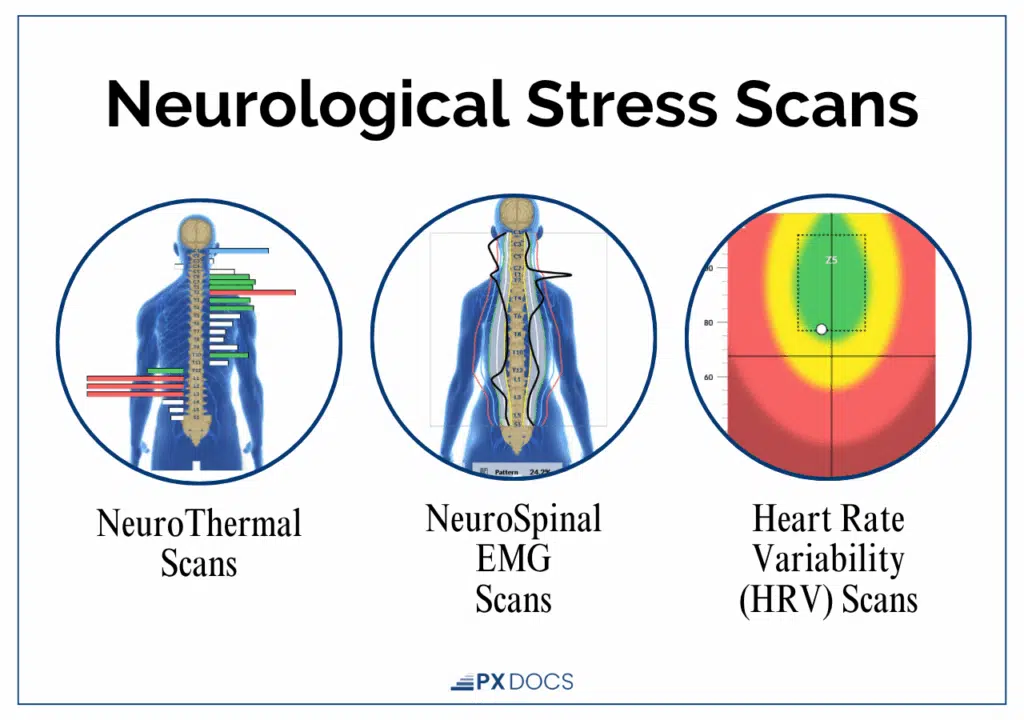
These non-invasive scans, safe for newborns, provide objective data about your child’s nervous system state. Children needing frequent antibiotics consistently show significant dysautonomia patterns, particularly in the upper cervical region. As care progresses, scans show the nervous system clearing, calming, and regulating—and parents report children stop getting sick as frequently.
This isn’t guesswork—it’s an objective measurement of nervous system change.
Supporting Your Child After Amoxicillin
While amoxicillin clears in 6-8 hours, its effects on gut bacteria persist much longer. Support recovery with:
- Probiotics: Give during treatment (2-3 hours apart from doses) and continue 2-4 weeks after. Choose pediatric formulations with Lactobacillus and Bifidobacterium species.
- Nutrition: Focus on prebiotic foods (bananas, oats, apples), anti-inflammatory foods, bone broth, fermented foods, and adequate hydration. Limit processed foods and sugar.
- Nervous System Support: Neurologically-Focused Chiropractic Care addresses subluxation and supports drainage and immune function. Prioritize sleep quality, reduce stress, and consider natural remedies for future infections.
The goal isn’t avoiding antibiotics when necessary—it’s building a nervous system resilient enough that antibiotics become the rare exception rather than the repeated rule.
When to Consult a Healthcare Provider
Report severe or persistent diarrhea, worsening symptoms despite antibiotics, allergic reactions, unusual bruising, or yellowing skin to your healthcare provider immediately.
Before accepting prescriptions, ask critical questions:
- “Are you certain this is bacterial rather than viral?”
- “What are the risks of watching and waiting 24-48 hours?”
- “Could this relate to underlying drainage or immune issues?”
- “Has my child had more than 2-3 antibiotic courses this year?”
Remember that antibiotics are necessary for true bacterial infections, but are overprescribed in children. Working with providers who understand both conventional medicine and root neurological causes gives your child the best chance for long-term health.
Breaking the Antibiotic Dependency Cycle
For too long, antibiotics have been treated as a first-line defense instead of a last resort. When used unnecessarily, the immune system, gut microbiome, and nervous system become weaker and more dysregulated.
The natural health philosophy understands that children occasionally experiencing colds and mild infections is normal. By overcoming these challenges naturally, through chiropractic adjustments and natural remedies, the immune system actually becomes stronger over time. Each infection overcome naturally trains immunity. This is the opposite of the antibiotic dependency cycle, where each course weakens natural immunity.
Promoting Optimal Health and Resilience
Navigating the use of antibiotics for your child can be challenging, but understanding how these medications work in the body and the factors that influence their duration can help you make informed decisions about your child’s care.
By working closely with healthcare providers, supporting your child’s overall health, and taking a comprehensive approach to wellness, you can help your child build resilience and thrive.
Remember, antibiotics are just one piece of the puzzle when it comes to promoting optimal health for your child. This isn’t about replacing antibiotics with wishful thinking; it’s about addressing why your child needed them repeatedly and giving their nervous system the support to function as designed.
Visit the PX Docs Directory to find a qualified pediatric chiropractor trained in neurologically-focused care who can develop a personalized plan for your child’s unique needs. Together, we can work toward a future where antibiotics are the rare exception rather than the repeated rule.ce vibrant, resilient health.