As a parent, you know when something isn’t quite right with your child. Maybe your little one has a persistent cough that just won’t go away, or they seem fussy and uncomfortable after eating.
You’ve taken them to the pediatrician, but you’re told it’s just a phase or a common childhood ailment. But what if there’s more to the story?
Silent reflux, also known as laryngopharyngeal reflux (LPR), is a condition that often goes unnoticed and undiagnosed in children. Unlike the more well-known gastroesophageal reflux disease (GERD), silent reflux in babies and children doesn’t always present with obvious symptoms like heartburn or vomiting. If left untreated, silent reflux can lead to more serious health issues and impact a child’s quality of life.
In this article, we’ll explore the causes, symptoms, and treatment options for silent reflux in children. We’ll also explore the unique approach of PX Docs, a network of Neurologically-Focused Pediatric Chiropractic specialists who work to address the root cause of this condition and restore balance to the nervous system.
What is Silent Reflux?
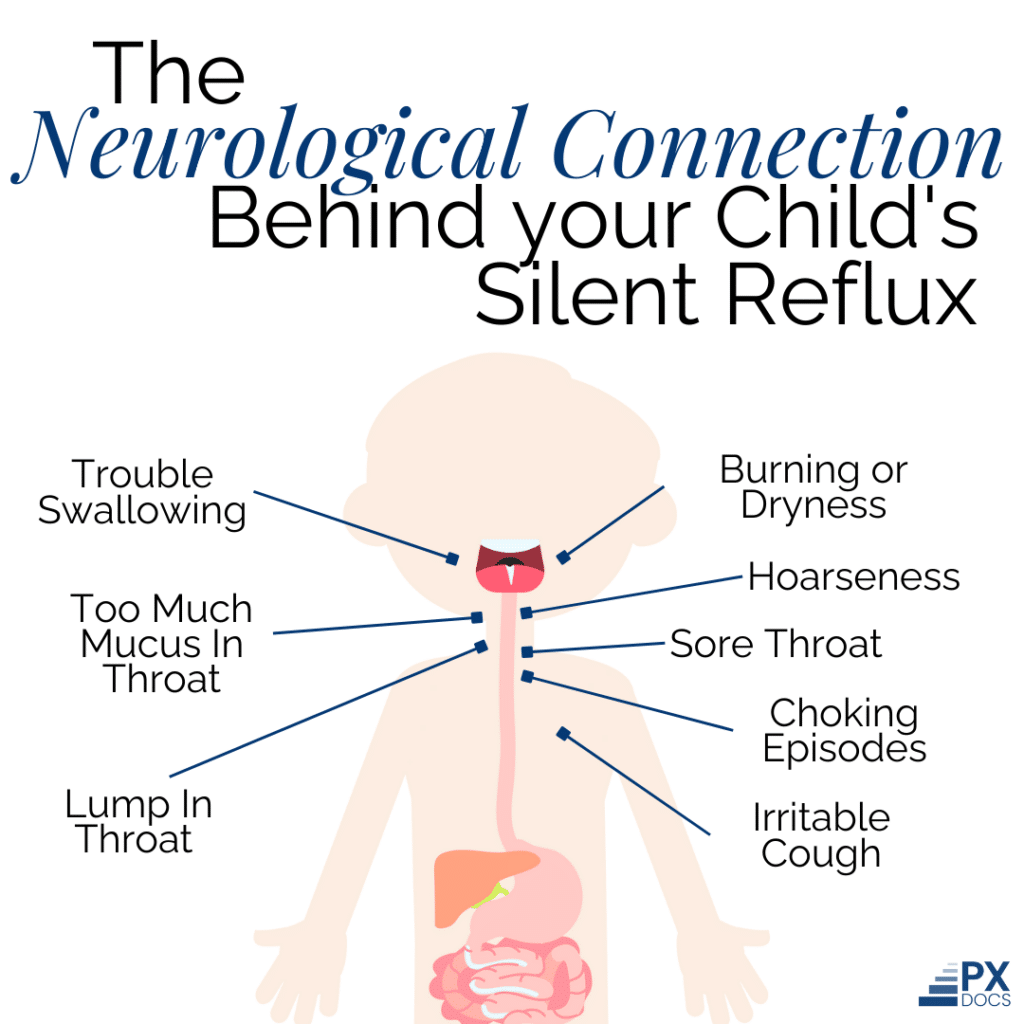
Silent reflux is a condition in which stomach contents flow back up into the throat and voice box (larynx). Unlike gastroesophageal reflux disease (GERD), which is characterized by heartburn and indigestion, silent reflux often doesn’t present with any noticeable symptoms in the chest or stomach area. This is why it’s called “silent” reflux.
To understand how silent reflux occurs, it’s helpful to know a bit about the anatomy of the digestive system. At the bottom of the esophagus, there is a ring of muscle called the lower esophageal sphincter (LES). The LES acts as a valve, opening to allow food and liquid to pass into the stomach and then closing to prevent stomach contents from flowing back up into the esophagus.
With silent acid reflux, however, the LES doesn’t work properly, allowing stomach acid to travel up the esophagus. The reflux can reach the throat and voice box, causing irritation and inflammation.
The dysfunction of this valve and muscle is not just random or bad luck, it’s likely caused by neurological interference and disrupted communication. All muscles, especially those that function in this manner, have sensory receptors that communicate with the brain and nervous system letting it know when to contract and when to relax. If there is subluxation or neuromuscular interference present, something very common in infants, then that interference can show up as this dysfunction and contribute to silent reflux.
Some other key differences between silent reflux (LPR) and GERD include:
- Location of symptoms: LPR affects the throat and voice box, while GERD primarily affects the lower esophagus and stomach.
- Type of symptoms: LPR symptoms are often related to the throat and voice, such as hoarseness, cough, and the sensation of a lump in the throat. GERD symptoms are more likely to include heartburn, chest pain, and regurgitation.
- Severity of reflux: LPR can occur with even small amounts of reflux, as the throat and voice box are more sensitive to stomach acid than the esophagus.
By understanding the underlying anatomy and differences between silent reflux and GERD, parents can better recognize the signs of silent reflux in their children and seek appropriate care.
Signs of Silent Reflux in Children
Silent reflux can be challenging to identify in children because the symptoms are often subtle and easily mistaken for other conditions. However, knowing what to look for can help parents recognize when their child may be experiencing LPR.
Some of the most common signs of silent reflux in children include:
- Hoarseness or a raspy voice
- Chronic cough or excessive throat-clearing
- Difficulty swallowing or the sensation of a lump in the throat
- Recurrent ear infections or fluid in the middle ear
- Chronic sinus infections
- Asthma-like symptoms, such as wheezing or trouble breathing
Over time, untreated silent reflux can lead to more serious complications in children. The constant backflow of stomach acid can cause inflammation and irritation in the throat and voice box, leading to conditions such as:
- Laryngitis: Inflammation of the voice box, which can cause hoarseness and loss of voice
- Subglottic stenosis: Narrowing of the airway below the vocal cords, which can lead to breathing difficulties
- Recurrent croup: A viral infection that causes swelling in the throat and voice box, which can be exacerbated by reflux
- Increased risk of respiratory infections, such as pneumonia or bronchitis
In addition to these physical complications, children with silent reflux may experience difficulties with feeding, sleeping, and overall quality of life. They may become fussy or irritable, refuse to eat, or have trouble gaining weight.
Causes of Silent Acid Reflux: Understand “The Perfect Storm”
While silent reflux can have various causes, the team at PX Docs has identified a common pattern of factors that they refer to as “The Perfect Storm.” This concept describes how a combination of prenatal, perinatal, and postnatal stressors can set the stage for the development of silent reflux and other health challenges in children.
One of the key elements of “The Perfect Storm” is prenatal maternal stress. When a mother experiences high levels of stress during pregnancy, it can impact the developing nervous system of the fetus. This can cause the baby’s nervous system to become “stuck” in a sympathetic dominant state, leading to a range of health issues, including silent reflux.
Another factor that can contribute to “The Perfect Storm” is birth interventions and trauma. Procedures such as c-sections, forceps deliveries, and vacuum extractions can cause physical injury on the delicate structures of the neck and throat. This can lead to a condition called subluxation, which involves dysfunction in the nervous system and can contribute to the development of silent reflux.
At the heart of “The Perfect Storm” concept is the idea of nervous system dysregulation. When the nervous system becomes imbalanced due to factors such as subluxation or early life stressors, it can affect the function of the digestive system and contribute to the development of silent reflux.
Some specific ways in which nervous system dysregulation can impact digestive function include:
- Impaired motility: When the nervous system is not functioning optimally, it can slow down food movement through the digestive tract, leading to reflux and other symptoms.
- Altered secretion: Dysregulation of the nervous system can affect the production and release of digestive enzymes and acid, leading to imbalances that can contribute to reflux.
- Inflammation: Chronic nervous system imbalance can lead to inflammation throughout the body, including in the digestive tract, which can exacerbate reflux symptoms.
Fortunately, by understanding the role of “The Perfect Storm” and nervous system dysregulation and subluxation in the development of silent reflux, parents can begin to see how a holistic, neurologically-focused approach to care may benefit their child.
Diagnosing Silent Acid Reflux
One of the challenges of silent reflux is that it can be difficult to diagnose, particularly in young children who may not be able to verbalize their symptoms. Unlike GERD, which often presents with more obvious signs like frequent spit-ups or heartburn, silent reflux can be more subtle and easily overlooked.
Typically, diagnosing silent reflux involves a combination of a thorough medical history, physical examination, and specialized testing. Some of the tests that may be used to diagnose silent reflux include:
- Endoscopy: This procedure involves inserting a small, flexible tube with a camera on the end into the throat and esophagus to visualize any signs of inflammation or damage.
- pH monitoring: This test measures the acidity level in the esophagus over a period of time to determine if reflux is occurring.
- Impedance testing: This test measures the movement of fluid and air through the esophagus to detect reflux episodes that may not be acidic enough to trigger symptoms.
While these tests can be helpful in confirming a diagnosis of silent reflux, they don’t always provide a complete picture of the underlying causes and contributing factors. This is where PX Docs’ unique approach comes in.
The INSiGHT Scans and Silent Reflux
So often for infants and children struggling with silent reflux, just going through the medical testing and diagnosis pathway for silent reflux adds more stress and tension to their delicate nervous system, actually making the condition worse. At PX Docs, we use non-invasive technology called the INSiGHT Scans that look deeper and find subluxation and nervous system dysfunction.
Below is a NeuroThermal scan of a child struggling with silent reflux. The green, blue, and red bars that go back and forth throughout this scan indicate subluxation and nervous system dysfunction, with the worst of it being centered right in that mid-thoracic region. This is the region of the nervous system that coordinates and stimulates stomach, pancreas, and other key digestive motility, absorption, and elimination functions. Therefore when it is significantly subluxated and dysfunction like shown in this child’s scan, we know that their digestion is going to be compromised and things like silent reflux often present as a result.
The PX Docs Approach to Managing Silent Reflux
Once a diagnosis of silent reflux has been made, the providers at PX Docs work with families to develop a comprehensive, individualized care plan to address the root causes of the condition. This approach is centered around the principles of Neurologically-Focused Chiropractic Care, which aims to restore balance and optimal function to the nervous system.
Neurologically-focused adjustments first aim to release stuck tension and sympathetic dominance, which is known to decrease digestive motility as well as the secretion of key enzymes. Adjustments also look to stimulate the vagus nerve and parasympathetic branch of the nervous system, which activate digestive motility, enzyme production, and so much more than helps address the root cause of silent reflux.
By the time many parents and patients have reached out for help in a PX Docs office they’ve already tried dietary changes, positioning changes, and even natural remedies such as certain herbs or supplements. Each of these things can help aid digestion, but so often the deeper root cause is nervous system dysregulation and sympathetic dominance, as discussed here throughout this article.
Beyond Symptom Management: Choosing Root-Based Care
Silent acid reflux can be a challenging and often overlooked condition in children. Fortunately, by understanding the underlying root causes of silent reflux, including the role of “The Perfect Storm” and nervous system dysfunction, parents can begin to see the importance of a holistic, neurologically-focused approach to care.
The providers at PX Docs are committed to helping families heal from silent acid reflux and other neurological imbalances. Through advanced technology and supportive lifestyle therapies, they work to address the root causes of dysfunction and restore balance to the nervous system.
If you suspect your child may be struggling with silent reflux or other health challenges, we encourage you to visit the PX Docs directory to find a qualified provider in your area. With the right support and care, your child can experience the joys of a happy, healthy childhood, free from the discomfort and limitations of silent reflux.