Do you find yourself constantly exhausted despite getting what should be enough sleep? Are you experiencing unexplained weight changes, mood swings, brain fog, or a seemingly endless cycle of stress?
What many conventional healthcare providers fail to recognize is that these signs may be traits of HPA axis dysfunction—a condition that affects the complex communication network between your hypothalamus, pituitary, and adrenal glands. This vital system regulates everything from your stress response and energy levels to immune function and metabolism.
While you may have heard the term “adrenal fatigue” to describe these signs, the reality may be more complex. The conventional approach often focuses on managing individual signs—prescribing medications for anxiety, addressing sleep issues separately, or recommending generic lifestyle changes—without identifying the underlying neurological imbalance at the root of these problems.
We recognize that these HPA axis dysfunction traits aren’t just isolated issues, but signs of a deeper nervous system dysregulation that affects this crucial hormonal communication pathway. By understanding how stress, inflammation, and nervous system imbalances impact the HPA axis, we can address the true root cause rather than merely masking the signs.
What is HPA Axis Dysfunction?
Hypothalamic-Pituitary-Adrenal (HPA) Axis dysfunction refers to an imbalance or dysregulation in the complex communication network between three critical components of the endocrine system: the hypothalamus, the pituitary gland, and the adrenal glands. HPA axis dysfunction is a complex problem, involving the entire stress-response system and its interconnections with the central nervous system.
This axis serves as a primary command center for stress regulation in the body, with each component playing a vital role:
- Hypothalamus: This region of the brain enables the body to maintain homeostasis by regulating body temperature, sleep, hunger, thirst, and emotions. When stress is detected, the hypothalamus secretes Corticotropin-Releasing Hormone (CRH).
- Pituitary Gland: Sometimes called the “master gland,” this tiny structure at the base of the brain receives CRH signals and responds by releasing Adrenocorticotropic Hormone (ACTH) into the bloodstream.
- Adrenal Glands: Small glands located atop each kidney that produce key hormones including cortisol, aldosterone, androgenic steroids (DHEA, testosterone), epinephrine (adrenaline), and norepinephrine (noradrenaline) in response to ACTH.
Under normal circumstances, these three components work in harmony to regulate your energy levels, mood, stress response, motivation, metabolism, and immune system. When you experience stress, this axis activates to help your body respond appropriately—increasing alertness, raising blood sugar for quick energy, and modulating inflammation. Once the stress passes, the system should return to baseline.
However, with chronic, prolonged stress—whether physical, emotional, or environmental—this delicate balance can become disrupted. Instead of adrenal glands simply “fatiguing,” the entire HPA axis can develop various patterns of dysfunction.
In some cases, cortisol production becomes erratic, with levels that may be inappropriately high at times when they should be low (like bedtime) or insufficient during times when they’re needed (like morning). In other cases, receptor sensitivity changes, meaning even normal hormone levels don’t produce appropriate responses in the body’s tissues.
What makes this condition particularly complex is that it involves much more than just hormone production. The HPA axis is intimately connected with the nervous system, especially the Autonomic Nervous System that controls our “fight-or-flight” and “rest-regulate-and-digest” responses. When subluxation and dysautonomia (dysfunction in the Autonomic Nervous System) are present, they can perpetuate and worsen HPA axis imbalances, creating a vicious cycle that conventional medicine often fails to recognize or address.
The “Perfect Storm” of Root Causes in HPA Axis Dysfunction
We often refer to the combination of factors that lead to chronic health conditions like HPA axis dysfunction as The “Perfect Storm.” This concept recognizes that health challenges rarely stem from a single cause but rather develop through a flow of interconnected stressors that overwhelm the body’s natural resilience over time.
The “Perfect Storm” for HPA axis dysfunction typically begins early in life, often before a child is even born. Prenatal stress plays a crucial role in setting the stage for future dysregulation. Research has shown that maternal stress during pregnancy can cause HPA axis dysfunction in the fetus.
Birth trauma represents another significant trigger for HPA axis dysfunction. Interventions such as forceps delivery, vacuum extraction, C-sections, and induction can cause physical trauma to an infant’s delicate neurospinal system, particularly affecting the upper cervical spine and brainstem region.
This area houses critical neurological structures involved in autonomic regulation, including pathways that influence the HPA axis. The physical strain from these interventions can create subluxation—areas of tension and neurological interference that disrupt proper communication between the brain and body, including the endocrine system that governs the HPA axis.
Beyond these early life factors, several ongoing stressors can contribute to HPA axis dysfunction:
- Chronic psychological stress from work, relationships, financial pressures, or constant digital connectivity keeps the stress response activated without adequate recovery periods
- Sleep disruption and circadian rhythm conditions that interfere with the normal daily cortisol rhythm
- Environmental toxins including mold, pollutants, pesticides, and endocrine-disrupting chemicals that challenge the body’s detoxification systems
- Inflammation from food sensitivities, gut dysbiosis, or autoimmune conditions that create physiological stress
- Undiagnosed infections that create ongoing immune system activation
- Medication use, especially antibiotics, corticosteroids, and hormonal contraceptives that can disrupt HPA axis function
The vagus nerve plays a particularly critical role in this process. This major nerve connects the brain to nearly every major organ and is a key component of the parasympathetic (“rest and digest”) nervous system.
When subluxation affects the areas where the vagus nerve originates, or when chronic stress suppresses vagal tone, it creates a state of dysautonomia—imbalance between the sympathetic and parasympathetic branches of the Autonomic Nervous System. This imbalance impacts HPA axis function, as the vagus nerve helps regulate the hypothalamus, which can initiate the entire HPA axis cascade.
Without addressing these interconnected root causes—particularly the neurological dysfunction that maintains this cycle—many people find themselves trapped in a downward spiral of worsening signs and declining health.
How HPA Axis Dysfunction Affects Your Health
HPA axis dysfunction can manifest in a surprisingly wide range of signs that might seem unrelated at first glance. This is because the HPA axis influences virtually every system in the body—from metabolism and immune function to mood regulation and cognitive performance. When this critical communication network becomes dysregulated, the effects can be far-reaching and debilitating.
The most common HPA axis dysfunction signs experienced by those with HPA axis dysfunction can be grouped into several categories:
Physical Signs:
- Persistent fatigue and exhaustion that isn’t relieved by sleep
- Disrupted sleep patterns (difficulty falling asleep, staying asleep, or waking unrefreshed)
- Unexplained weight changes (either gain or loss)
- Weakened immune function leading to frequent infections
- Digestive issues including constipation, diarrhea, bloating, and IBS-like traits
- Changes in blood pressure (either high or low)
- Dizziness upon standing (orthostatic hypotension)
- Poor circulation and feeling “puffy”
- Weak nails and hair loss
- Salt and sugar cravings
Cognitive and Emotional Signs:
- Brain fog and difficulty concentrating
- Memory problems
- Increased anxiety and worry
- Depressed mood
- Irritability and mood swings
- Poor stress tolerance
- Feeling “wired but tired” (especially at night)
- Light sensitivity
- Decreased motivation
Hormonal Imbalances:
- Changes in menstrual cycle (irregular periods, heavier/lighter flow)
- Low libido
- Fertility challenges
- Thyroid dysfunction traits
- Blood sugar regulation issues
What makes this dysfunction particularly challenging is the way signs can create a vicious cycle. For example, the fatigue leads to reduced physical activity, which worsens sleep quality, which further impacts HPA axis function, which increases inflammation, which creates more fatigue.
Testing for HPA Axis Dysfunction
Accurate assessment of HPA axis function is essential for developing an effective care approach. Unfortunately, conventional medical testing often misses the subtle imbalances that characterize HPA axis dysfunction. Standard blood tests typically measure hormones at single points in time, failing to capture the dynamic patterns that define this condition.
More comprehensive testing approaches can provide deeper insights into HPA axis function:
- Salivary cortisol testing: This method measures cortisol levels at multiple points throughout the day (typically morning, noon, afternoon, and evening), revealing the daily cortisol rhythm rather than just a single snapshot. This pattern is often more informative than absolute levels.
- DUTCH testing (Dried Urine Test for Comprehensive Hormones): This advanced testing method provides detailed information about cortisol production, metabolism, and metabolites, offering insights into both the quantity and quality of hormone production.
- Adrenocortex Stress Profile: This test measures cortisol and DHEA (another important adrenal hormone) through carefully timed saliva samples, helping to identify specific patterns of HPA dysfunction.
- Heart Rate Variability (HRV) assessment: HRV provides a window into Autonomic Nervous System function, which is closely linked to HPA axis regulation. Low HRV is often associated with HPA axis dysfunction and chronic cortisol release.
While these specialized tests can provide valuable information, at PX Docs, we recognize that testing alone isn’t enough.
The PX Docs Approach to Healing HPA Axis Dysfunction
Neurologically-Focused Chiropractic Care offers an approach to HPA axis dysfunction by focusing on the intricate relationship between the nervous system and the HPA axis. This approach recognizes that subluxation—areas of tension, and neurological interference in the spine—can disrupt the critical communication pathways between the brain and body, including those that regulate the stress response.
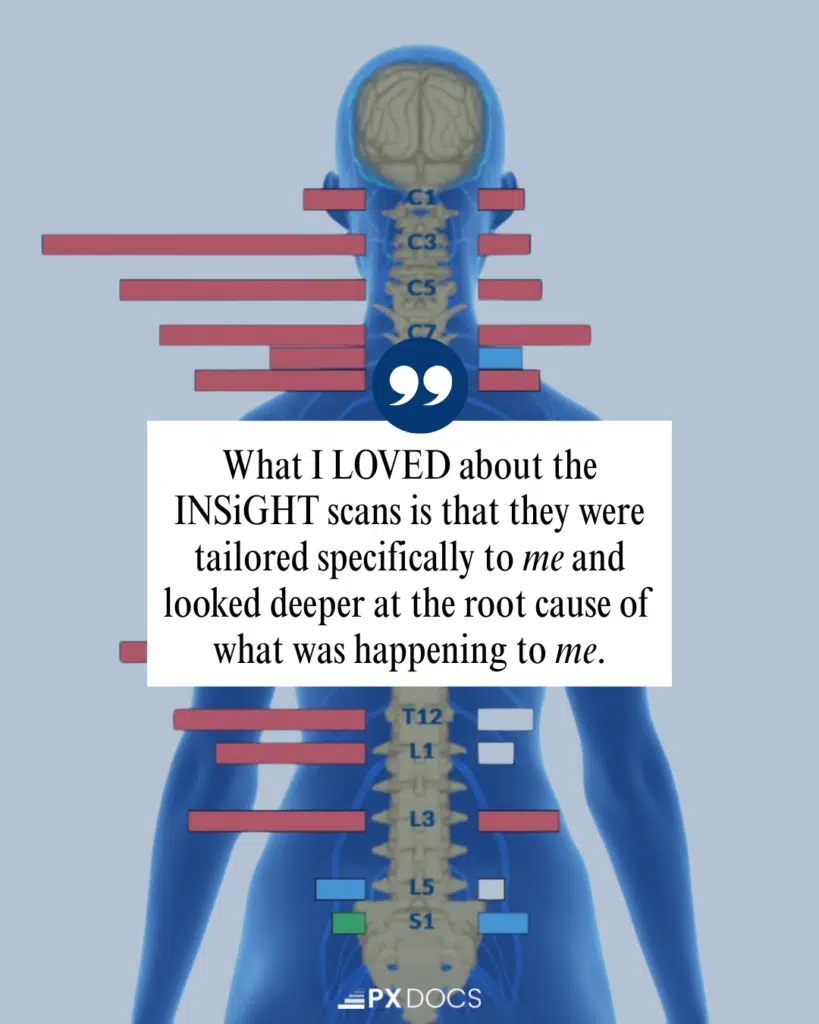
That’s why our approach incorporates INSiGHT Neurological Scanning, a non-invasive assessment that helps identify the underlying neurological imbalances contributing to HPA axis dysfunction.
The INSiGHT Scans consist of three components that provide crucial information about nervous system function:
- NeuroThermal Scanning: Detects patterns of autonomic disturbance along the spine that may affect HPA axis regulation
- NeuroSpinal EMG: Measures tension patterns in the muscles supporting the spine, which can indicate areas of neurological stress and subluxation
- Heart Rate Variability Assessment: Evaluates the balance between sympathetic and Parasympathetic Nervous System function, which directly impacts HPA axis regulation
These scans allow PX Docs practitioners to identify specific patterns of neurological dysfunction and create customized care plans that address the unique root causes of each individual’s HPA axis dysfunction.
Supportive Strategies for Recovery
While addressing the neurological component of HPA axis dysfunction is essential, a comprehensive approach that includes supportive lifestyle strategies can accelerate healing and improve outcomes. These strategies work synergistically with Neurologically-Focused Chiropractic Care to restore balance to the HPA axis and improve overall well-being.
Nutrition Support
The HPA axis requires specific nutrients to function optimally. During periods of chronic stress, these nutrients are often depleted, further compromising HPA axis function. Key nutrients that support HPA axis recovery include:
- Vitamin C: Essential for adrenal hormone production and a key antioxidant for protecting these glands
- Magnesium: Helps regulate the stress response and is rapidly depleted during chronic stress
- B vitamins: Critical for energy production and nervous system function
- Omega-3 fatty acids: Support healthy inflammation response and brain function
Blood Sugar Regulation
Insufficient blood glucose can negatively affect the HPA axis through the Paraventricular Nucleus (PVN). Stabilizing blood sugar through regular meals containing protein, healthy fats, and complex carbohydrates helps reduce this stress and supports recovery. Specific strategies include:
- Starting the day with 25-30 grams of protein
- Including healthy fats and fiber with meals
- Limiting refined carbohydrates and sugar
- Avoiding caffeine until after breakfast
- Having balanced snacks if needed to prevent drops in blood sugar
Stress Reduction Techniques
Since chronic stress can lead to more than one form of HPA axis dysfunction, incorporating stress reduction practices is essential. Effective approaches include:
- Regular mindfulness meditation or breathing practices
- Gentle movement like yoga or tai chi
- Time in nature
- Boundaries around work and digital connectivity
- Scheduling regular downtime and recovery periods
Sleep Optimization
Quality sleep is crucial for HPA axis recovery. Supporting healthy sleep patterns includes:
- Maintaining consistent sleep and wake times
- Creating a dark, cool, quiet sleep environment
- Limiting screen time before bed
- Supporting healthy circadian rhythms through morning sunlight exposure
- Considering sleep-supportive nutrients or herbs if needed
Adaptogenic Herbs
Certain herbs known as adaptogens can help support healthy HPA axis function. These herbs help the body respond more effectively to stress and may support resilience. Common adaptogens include ashwagandha, rhodiola, holy basil, eleuthero, and schisandra. These should be used under professional guidance, ideally as part of a comprehensive approach rather than in isolation.
It’s important to note that these supportive strategies are most effective when combined with addressing the underlying neurological imbalances through Neurologically-Focused Chiropractic Care. This approach addresses both the root causes and the contributing factors of HPA axis dysfunction, providing the foundation for sustainable healing.
Reclaiming Balance and Vitality
Hypothalamic-Pituitary-Adrenal (HPA) Axis dysfunction represents a complex interplay between your nervous system, endocrine system, and the cumulative effects of various stressors throughout life. While conventional approaches often focus on managing individual signs or providing temporary relief, true healing requires addressing the root neurological causes that maintain this dysfunctional pattern.
By addressing these foundational aspects of neurological health, we help restore the communication pathways that allow your body’s natural healing abilities to function optimally. Recovery from HPA axis dysfunction is not an overnight process. The same systems that took months or years to become dysregulated require time and consistent support to rebalance.
We invite you to visit the PX Docs Directory to find a qualified Neurologically-Focused Chiropractor in your area who can help you begin your journey toward restored balance, improved resilience, and renewed vitality.
Your body has an incredible capacity to heal when given the right support—take the first step today toward reclaiming your health and well-being.